
Obesity can take up to 14 years off your life.
So, instead of living to the average US life expectancy of your mid-70s, you would be expected only to live until you are 60 years old if you are severely obese. The average age of retirement in the USA is 65 years old.5
America is facing an epidemic. 1/3 of all Americans are obese (BMI >30), and it’s predicted that in 2030, over half of all Americans will be obese. With only 1 in 5 Americans not being overweight or obese.1,2
As a %, we are the 10th fattest country in the world. We are #1, the winner, of high GDP countries. That means, even though we have more money per person than most other countries, no other rich country comes even close to our obesity numbers.3,4
What the f*** is going on here?
Obesity kills us quicker, makes our lives worse, and costs tons of money.
Numerically, this could mean 14 years off your life, a potentially 55% increased risk of anxiety and depression, and contributing to a whopping 20% of all of the USA’s healthcare costs.5-7
And here’s why I care: it’s preventable. After smoking, obesity is the second leading cause of preventable deaths in America.
Is it the food? Genetics? Our activites?
The US government has tried to help but has failed. I simply don’t think enough time and money has gone into prevention, with only maybe ~$1 Billion being spent on preventative programs.
At the same time, obesity-related health care is costing the US 100x that at ~$100 Billion dollars spent on obesity-related healthcare, with that number only rising. Oh, and all those prevention programs? Mostly dismal failures. With only 1/5 having even somewhat positive results.9-10
I’ll repeat it: what the f*** is going on here? What can be done? How can we prevent 80% of the population from suffering an early, depressed, and poor demise by 2030?
In this post you’ll learn:
- The danger of normal American food
- The scary average activity of Americans
- How to fix it

1. The Food
It seems our food is bigger, more processed, and sweeter than anywhere else in the world. Many epidemiologists, doctors, and societies think food might be the reason why more and more people in the US are fat.
Also, throughout this post, I will say overweight (BMI > 25), obese (which means BMI >30), severely obese (BMI >40), and central obesity (weight circumference > 40 inches) .11 BMI is somewhat antiquated, with central obesity being currently being argued to correlate more accurately with health effects. Multiple reviews, however, conclude that once humans hit a BMI of >30, and especially >40, their are serious health consequences.12
Portions
Bigger is not better.
I see this every day. Have you bought an ice cream recently? Or a soda at a movie theater or fast food chain? The small is huge, and the large sizes border on hilarity.
In one study, researchers went to my hometown, Philadelphia, bought common foods, and then compared the portion sizes to those in Paris.
- Chinese food, 72% larger
- Candy bar, 41% larger
- Soft drink, 52% larger
- Hot Dog, 63% larger
- Yogurt, 82% larger
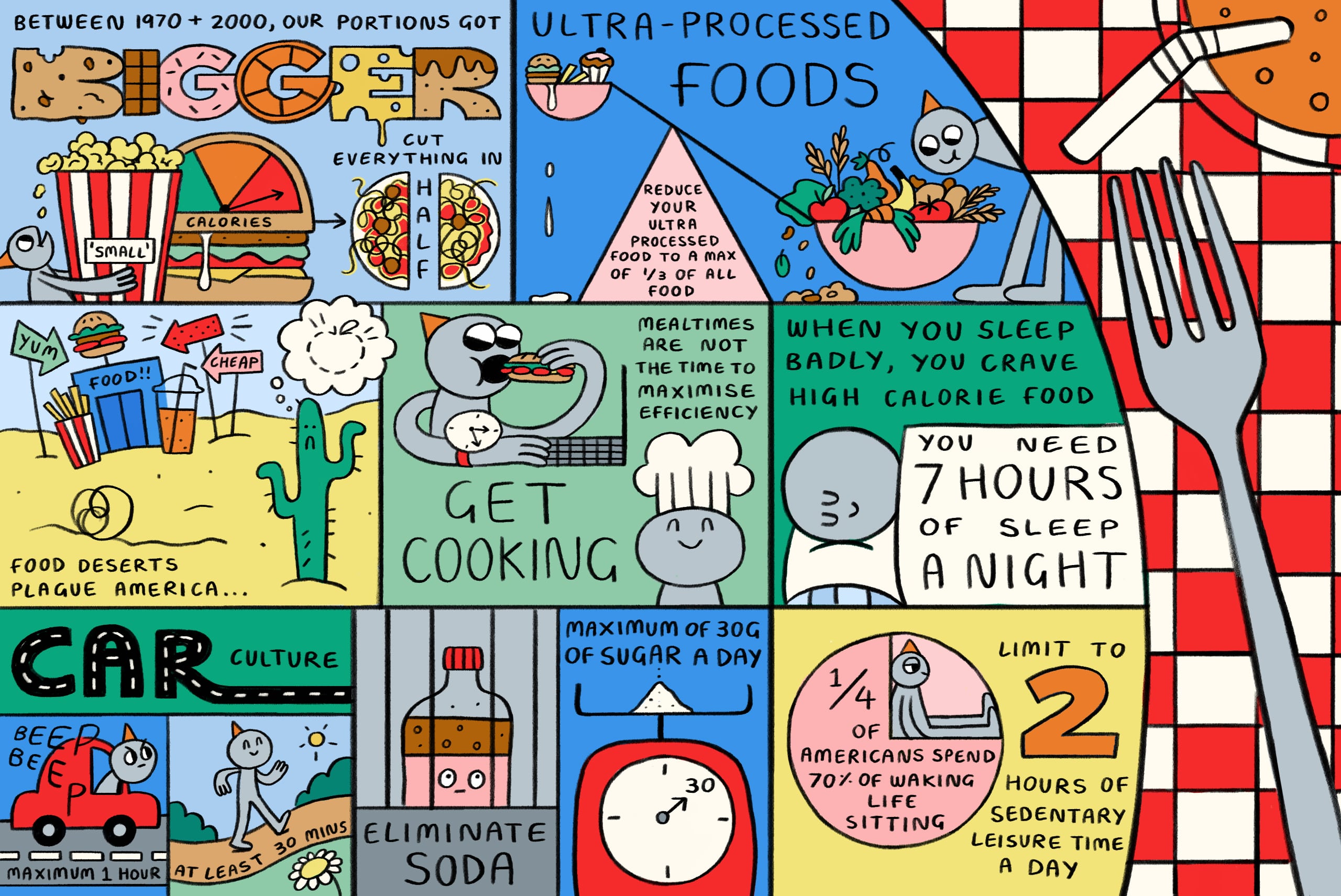
Between 1970 and 2000, something happened: Our portions got bigger—like way bigger.16 Oh, and we did, too.
The average calories in a hamburger have gone from 300 to 500. Two slices of pizza from 500 to 800, and the cup of coffee is the most staggering: from 8 oz with milk and sugar at 45 calories to 16 oz with various syrups and mochas and who-knows-what at 350 calories, that’s nearly a 10x increase in calories in a drink 2/3 of Americans drink.
I want to show you two crazy graphs from source 16, and this is from the year 2000, keep in mind:
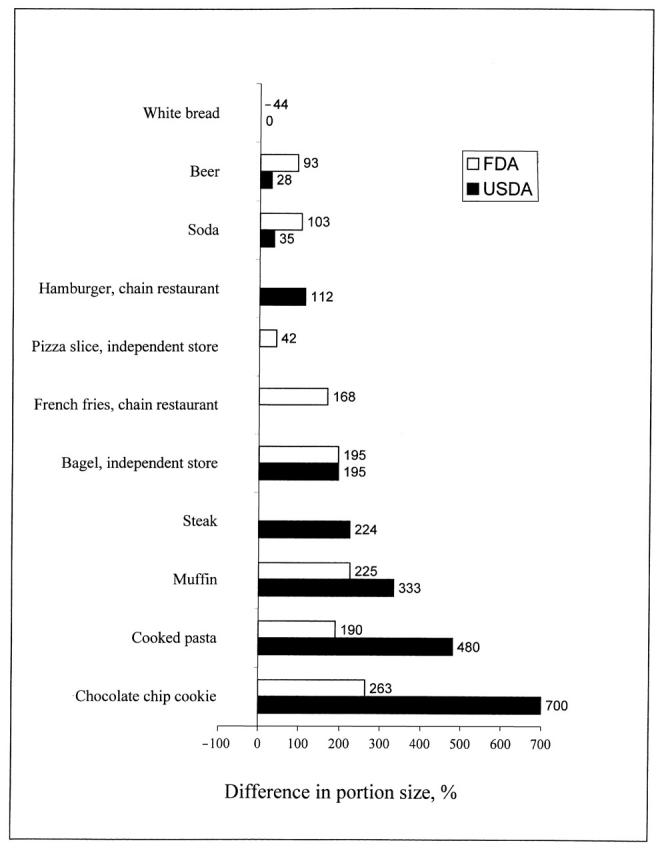
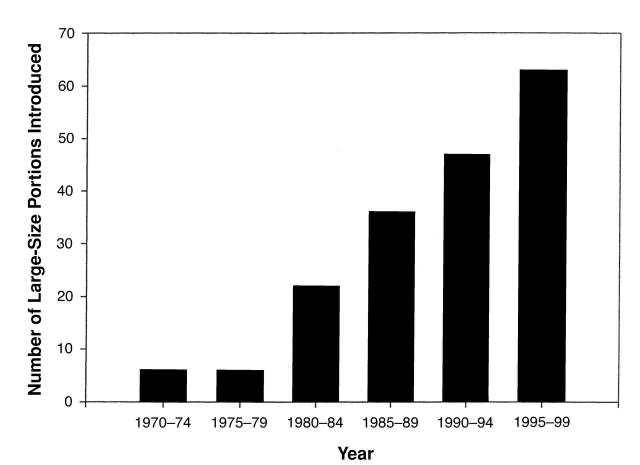
What happened in the 80s and 90s? Remember that documentary about supersizing? That. That happened. Oh, and that guy is dead.
This alone could be the answer. If we are eating 1.5-2x as much food, it makes sense that we are 1.5x-2x bigger, and, interestingly, right around the time these food increases began, the obesity epidemic in America started. Between the 1970s and 1980s, the obesity rate of adults tripled (from 13% to 34%) and in children (from 5% to 17%).13-15
How to fix it: We (that means you) need to start serving and eating reasonable portions. Based on the above data, if you are obese, that means cutting pretty much everything in half. Sure, you can measure your cups, weigh the food, or count calories (you’ll be amazed at how many calories are in things), but if we want to be as thin as we were as a country in the mid-20th century or the majority of the rest of the world now, cut it in half.
Okay, I must move on, or this will be a 300-page article. Let’s talk about processing.
Processing
The more processed your food is, the greater your chance of being obese, having cardiac disease, and having metabolic disease. Nice!17
Here is where I definitely mess up.
I eat troughs of packaged food, don’t cook for myself nearly enough, and have DoorDash as one of my most used Apps. Now, I’m genetically lucky, but I also exercise and try to control the amount of food I eat, so my BMI is right around 24/25. What I need to do better is control the type of food I eat, or I will likely face these same cardiac and metabolic issues regardless of my weight.
The NOVA classification, which isn’t an acronym but means “new” in Portuguese, classifies food into four groups:
- 1: Unprocessed food/minimally processed food – veggies, rice, meat, water, coffee, dried fruit, etc.
- 2: Oils/Fats/Sugar – self-explanatory.
- 3: Processed – bacon, fresh cheeses, canned or bottled vegetables with vinegar or salt, canned fish, beer/wine/cider, and similar items.
- 4: Ultra-processed – biscuits, ice cream, cookies, packaged bread, sweetened juices, cake, distilled alcohol, breakfast cereals and bars, pre-prepared burgers and hotdogs and “nuggets,” energy or sports drinks, and things like this.
I don’t even need to say anything. You can look at groups 1-4 yourselves and imagine how you would feel if you only ate from group 4 for a week versus group 1.
58% of US calories consumed are ultra-processed, and 36% in France.17
In one Spanish study, when comparing consumption of ultra-processed food, those in the top quartile of ultra-processed consumption were 26% more likely than those in the bottom quartile to be obese.18
How to fix it: Reduce your ultra-processed food consumption to a max of 1/3 of all food, and maximize group 1 foods.
Sugar
The US wins again! We are the biggest consumer of sugar around the world, at about 126 grams per day per person, while countries like India only consume 5 grams per person per day.
There is much controversy here as to the contribution of sugar to obesity. However, most of the controversy is industry vs. academia. A review article from 2015 says:
There are epidemiological data, plausible mechanisms and clinical data from diet intervention studies that provide strong support for a direct causal/contributory role of sugar in the epidemics of metabolic disease, and for an indirect causal/contributory role mediated by sugar consumption promoting body weight and fat gain. […] The controversy is further fueled by industry-funded studies that report that there are no adverse effects of consuming beverages containing up to 30% Ereq sucrose or HFCS (high fructose corn syrup) and by the null conclusions of recent meta-analyses.
Kimber L. Stanhope 2015
What most doctors seem to agree on is that sugar likely isn’t the only cause of the obesity epidemic but a definite contributor to weight gain.
In one notable study from the Lancet, they found that for every single sugar sweetened beverage (soda) a person drinks a day, their chances of obesity increase by 60%. So, if you even drink two sodas a day, you are more than twice as likely to be obese than someone who does not.20
How to fix it: Avoid ADDED sugar. For the love that all is holy, please try eliminating sugary sodas from your diet. Try to max out 30 grams of added sugar per day (you hit that with one soda, for your information). Try to reduce the consumption of diet sodas. Unfortunately, diet sodas aren’t that much better. What about sparkling water, or, please don’t strike me down, regular water?
For me, mostly removing soda and TV has dramatically improved my life since I was 16 years old. Of course, limiting cakes and sweets is also beneficial, but I think you can go too far here. I love a good hot fudge brownie sundae or waffle. What is life without a bit of whipped cream? I try to limit those to 1-2 days a week and never drink soda.
Overall, my fix for American obesity would be:
- Cut portions in half
- Shift ultra-processed food consumption from 2/3 of calories to 1/3
- Max at 30 g of added sugar a day
2. The Lifestyle
It’s not just the food…
We are more sedentary, sleep-deprived, and stressed than ever before.
Sedentary
Just take a second and think about how long you sat yesterday, at home, in your car, at work. Was it 8 hours? More?
American society is constantly being re-engineered to move as little as possible andles as possible. But this isn’t our bodies; human society has advanced so mind-bendingly use as few musc fast that evolution could in no way keep up.
Our bodies weren’t designed to sit for these extended periods of time. They evolved to perform manual labor constantly, whether that was hunting, foraging, running, or building we were working.
We have to focus on obesity here, or, again, this will become more of a textbook than an article.
However, this sedentary lifestyle isn’t great for cardiac, metabolic, and mental health. I dive deep into this in a post here aptly named “The Magic of Exercise.”
1/4 of Americans spend 70% of their waking hours sitting and virtually never exercise, so they are classified as sedentary.25 Not only that, when we finish work, we nearly always sit on a couch, in front of a computer, or in front of a TV.
Importantly, however, not just adding exercise but reducing sedentary activities might be the most impactful change:
Independent of exercise levels, sedentary behaviors, especially TV watching, were associated with significantly elevated risk of obesity and type 2 diabetes, whereas even light to moderate activity was associated with substantially lower risk.
Hu et. al., 200326
Light and moderate activity is, for example, waking slowly or briskly.
Movement feels so good, I feel bad for people that live like this.
How to fix it: Limit yourself to 2 hours of sedentary leisure activity a day. Aim for at least 30 minutes of exercise a day, no matter what. This could even be walking outside while in a phone meeting. The NIH also strongly recommends muscle-strengthening activities, like lifting weights, at least twice per week.
Sleep and Stress
When you sleep poorly, your body thinks a stressful time is coming. Evolutionarily, it’s like you are running away from a lion or competing tribe, so it releases more hormones to make you eat more (like more ghrelin and less leptin) because it wants to store up food in case because of this stressful event you won’t be eating a lot in the future. But very few of us today, and virtually no one in America, is running away from lions or warring with competing tribes. But our body still makes ghrelin and reduces leptin, which increases our appetite and makes us crave high-calorie foods.
In one randomized controlled trial, which is one of the best forms of testing a scientific hypothesis we have, those who slept 5.5 hours versus 8 hours ate 300 more calories per day, usually from late night snacking, than those who slept 8 hours.27
How to fix it: Get 7 hours of continuous sleep every night. If you can’t, understand that your body will make it much more difficult for you to resist high-calorie junk food because it’s gone into evolutionary stress overdrive.
3. The State of the Union
Finally, America’s infrastructure is not helping us. The lack of easy access to fresh fruits, vegetables, and meat, the food delivery boom, and our car-centric culture sacrifice health for speed.
Food Deserts
Food deserts plague America. In many low-income areas, it is simply cheaper to eat fast food. These people don’t have cars, and grocery stores are over a mile away, making it nearly impossible to access fresh food. Therefore, poverty-stricken areas are much more likely to be obese.28
Instant Gratification
Over 50% of American adults eat out three or more times a week, and over 35% eat fast-food meals more than twice a week. According to the CDC, the food we eat out is nearly always higher in calories, contributing to weight gain.
The culture around food is frankly awful in America when compared to most other developed countries. We don’t sit nearly as long at meals, aren’t with our family and friends, and don’t enjoy our meal-time.
The differences are astounding compared to Italy’s or Argentina’s average lunch or dinner. More people sit at the table, bring home-cooked food, or talk and enjoy each other’s company. In America, we are focused on efficiency, efficiency, efficiency, eating as fast as possible so we can move on to the next thing. But sitting down for a meal with loved ones is not one of these places we should be trying to maximize our efficiency.
The hour saved by stuffing a sandwich into our faces while walking, in a Zoom meeting, or talking on the phone is not worth it. We would benefit so much more by taking the hour to step back, sit down, and enjoy our limited time with the people we love.
How to fix it: aim for a maximum of three delivery or eating out occurrences per week. Phone my friend Gordon Ramsay up and get to cooking! Just make sure it’s not raw.
Car Centric Culture
When was the last time you tried to walk somewhere when you weren’t in a city in America?
In rural America, the suburbs, and even many cities, are not designed with pedestrians in mind. Not to mention public transport, which is only used by about 5% of Americans. Check out my friend’s YouTube channel, Notjustbikes, if you want to learn more.
One fantastic study looked at 10,000 people in Atlanta, Georgia. They found that for every additional hour spent in the car was assosciated with a 6% increase in the likelihood of obesity, while each additional kilometer walked per day was associated with a 5% decrease in the likelihood of obesity.30
How to fix it: Try to max out at an hour in the car every day and min out at 30 minutes of walking every day. Depending on your work and personal life, it may be hard, but it could also save your life.
Summary
The laws of thermodynamics hold. In hermetically sealed studies, where calories in and out are strictly tracked, people gain weight if they are in a calorie surplus and lose weight if they are in a calorie deficit, regardless of genetics. When people burn more calories than they consume, they lose weight. And when they consume more calories than they burn, they gain weight. Nothing in genetics can make someone stay overweight if they have a calorie deficit. Finally, macronutrient composition, so fat or protein or carb portion breakdown of the food, doesn’t matter for weight loss or gain either.22,23
However, what drives people to consume more or fewer calories and burn greater or fewer calories is hugely complicated and is heavily influenced by genetics and the environment. This is why the obesity epidemic in America is multifactorial and complex.
In America, we are losing big. There is a gargantuan amount of low-quality food and not enough movement, and we are trying to be efficient at everything without realizing the cost to our happiness and health.
The WHO has declared obesity a global epidemic, with nearly 1/5 of the entire world being obese. By 2060, this could cost the world $18 trillion, which is 1/5 of the world’s current GDP.
What can we do? Well, based on the current evidence, to live longer and be happier, we need to be less obese as a nation. To do that:
- Control portion size (cut it in half).
- Eat less ultra-processed (NOVA 4) food and more minimally processed food (NOVA 1); max at 33% of your calories from NOVA 4 daily.
- Try to eliminate added sugar as much as possible. Eliminate all soda and limit added sugar to 30 g per day.
- Avoid a sedentary lifestyle at all costs, max out your sedentary leisure time at 2 hours, and get at least 30 minutes of exercise daily.
- Avoid poor sleep and stress. It’s easy, right? Aim for 7 hours of sleep at a minimum, and try to remove stress-causing things from your life while adding stress-reducing things.
- If you can, move to a place where you walk more and drive less, it could save your life.
Wow, if you made it to the end of the post, well done! It shows you are well on your journey to improving your life and maybe making a global impact.
If you enjoyed this post, please share it with friends/family so we can all try to live happier and healthier lives.
Work Cited:
- https://www.cdc.gov/obesity/php/data-research/adult-obesity-prevalence-maps.html#:~:text=Across%20states%20and%20territories,and%20the%20Northeast%20(28.6%25).
- Wang Y, Beydoun MA, Min J, Xue H, Kaminsky LA, Cheskin LJ. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020 Jun 1;49(3):810-823. doi: 10.1093/ije/dyz273. PMID: 32016289; PMCID: PMC7394965.
- https://data.worldobesity.org/rankings/
- https://www.worldometers.info/gdp/gdp-per-capita/
- Kitahara CM, Flint AJ, Berrington de Gonzalez A, Bernstein L, Brotzman M, MacInnis RJ, Moore SC, Robien K, Rosenberg PS, Singh PN, Weiderpass E, Adami HO, Anton-Culver H, Ballard-Barbash R, Buring JE, Freedman DM, Fraser GE, Beane Freeman LE, Gapstur SM, Gaziano JM, Giles GG, Håkansson N, Hoppin JA, Hu FB, Koenig K, Linet MS, Park Y, Patel AV, Purdue MP, Schairer C, Sesso HD, Visvanathan K, White E, Wolk A, Zeleniuch-Jacquotte A, Hartge P. Association between class III obesity (BMI of 40-59 kg/m2) and mortality: a pooled analysis of 20 prospective studies. PLoS Med. 2014 Jul 8;11(7):e1001673. doi: 10.1371/journal.pmed.1001673. PMID: 25003901; PMCID: PMC4087039.
- Blasco BV, García-Jiménez J, Bodoano I, Gutiérrez-Rojas L. Obesity and Depression: Its Prevalence and Influence as a Prognostic Factor: A Systematic Review. Psychiatry Investig. 2020 Aug;17(8):715-724. doi: 10.30773/pi.2020.0099. Epub 2020 Aug 12. PMID: 32777922; PMCID: PMC7449839.
- Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK.. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring, Md) 2008;16:2323–330. [PubMed] [Google Scholar] [Ref list]
- Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: the skinny on interventions that work. Psychol Bull. 2006 Sep;132(5):667-91. doi: 10.1037/0033-2909.132.5.667. PMID: 16910747; PMCID: PMC1876697.
- Wolf AM. What is the economic cost for treating obesity? Obesity Research. 1998;6s:2. [PubMed] [Google Scholar] [Ref list]
- Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: the skinny on interventions that work. Psychol Bull. 2006 Sep;132(5):667-91. doi: 10.1037/0033-2909.132.5.667. PMID: 16910747; PMCID: PMC1876697.
- https://www.ncbi.nlm.nih.gov/books/NBK279167/
- https://www.ncbi.nlm.nih.gov/books/NBK594362/#:~:text=BMI’s%20association%20with%20health%20risk,%2C%20disease%20risks%2C%20or%20functionality.
- Rozin P, Kabnick K, Pete E, Fischler C, Shields C. The ecology of eating: smaller portion sizes in France Than in the United States help explain the French paradox. Psychol Sci. 2003 Sep;14(5):450-4. doi: 10.1111/1467-9280.02452. PMID: 12930475.
- https://www.ncbi.nlm.nih.gov/books/NBK44656/#:~:text=The%20prevalence%20of%20extreme%20obesity,in%20experiencing%20an%20obesity%20epidemic.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5359369/
- Young LR, Nestle M. The contribution of expanding portion sizes to the US obesity epidemic. Am J Public Health. 2002 Feb;92(2):246-9. doi: 10.2105/ajph.92.2.246. PMID: 11818300; PMCID: PMC1447051.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5787353/
- Mendonca RD, Pimenta AM, Gea A, de la Fuente-Arrillaga C, Martinez-Gonzalez MA, Lopes AC, et al. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-Up (SUN)cohort study. Am J Clin Nutr. 2016;104(5):1433–40. doi: 10.3945/ajcn.116.135004. This investigation is the first prospective cohort to examine the association between ultra-processed food consumption and incident overweight/obesity. Highly-educated middle-aged Spanish adults in the highest quartile of ultra-processed food intake at baseline had a 26% higher risk of developing overweight/obesity over a mean of 9 years of follow-up than those in the lowest quartile.
- Walton J, Bell H, Re R, Nugent AP. Current perspectives on global sugar consumption: definitions, recommendations, population intakes, challenges and future direction. Nutr Res Rev. 2023 Jun;36(1):1-22. doi: 10.1017/S095442242100024X. Epub 2021 Aug 9. Erratum in: Nutr Res Rev. 2023 Jun;36(1):177-178. doi: 10.1017/S0954422422000075. PMID: 34369326.
- Stanhope KL. Sugar consumption, metabolic disease and obesity: The state of the controversy. Crit Rev Clin Lab Sci. 2016;53(1):52-67. doi: 10.3109/10408363.2015.1084990. Epub 2015 Sep 17. PMID: 26376619; PMCID: PMC4822166.
- Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357:505–8. [PubMed] [Google Scholar][Ref list]
- Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, McManus K, Champagne CM, Bishop LM, Laranjo N, Leboff MS, Rood JC, de Jonge L, Greenway FL, Loria CM, Obarzanek E, Williamson DA. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009 Feb 26;360(9):859-73. doi: 10.1056/NEJMoa0804748. PMID: 19246357; PMCID: PMC2763382.
- https://www.ncbi.nlm.nih.gov/books/NBK221839/
- Owen N, Sparling PB, Healy GN, Dunstan DW, Matthews CE. Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc. 2010 Dec;85(12):1138-41. doi: 10.4065/mcp.2010.0444. PMID: 21123641; PMCID: PMC2996155.
- Owen N, Sparling PB, Healy GN, Dunstan DW, Matthews CE. Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc. 2010 Dec;85(12):1138-41. doi: 10.4065/mcp.2010.0444. PMID: 21123641; PMCID: PMC2996155.
- Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television Watching and Other Sedentary Behaviors in Relation to Risk of Obesity and Type 2 Diabetes Mellitus in Women. JAMA. 2003;289(14):1785–1791. doi:10.1001/jama.289.14.1785
- Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD. Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr. 2009 Jan;89(1):126-33. doi: 10.3945/ajcn.2008.26574. Epub 2008 Dec 3. PMID: 19056602; PMCID: PMC2615460.
- Hedwig Lee, Megan Andrew, Achamyeleh Gebremariam, Julie C. Lumeng, and Joyce M. Lee, 2014. Longitudinal Associations Between Poverty and Obesity From Birth Through AdolescenceAmerican Journal of Public Health 104, e70_e76,https://doi.org/10.2105/AJPH.2013.301806
- Ju SY. Changes in Eating-Out Frequency according to Sociodemographic Characteristics and Nutrient Intakes among Korean Adults. Iran J Public Health. 2020 Jan;49(1):46-55. PMID: 32309223; PMCID: PMC7152649.
- Frank LD, Andresen MA, Schmid TL. Obesity relationships with community design, physical activity, and time spent in cars. Am J Prev Med. 2004 Aug;27(2):87-96. doi: 10.1016/j.amepre.2004.04.011. PMID: 15261894.

3 comments
Amy
Great essay, Zach! Did you make that adorable and awesome drawing above the section about food?
Zach
Thanks Amy! No that’s my amazing Illustrator Rosa, you can see her stuff here: https://rosafisher.co.uk
Amy
Word! Will do!
Keep fighting the good fight.