Evidence-Based Health 101
Your Step-by-Step Guide to Becoming a Healthier Human Based on Evidence
5-Min Health ROI Calculator⬇️ Jump to the list of Articles ⬇️This framework represents the synthesis of thousands of studies, millions of participants, and decades of health economics research into a systematic approach that treats health decisions with the rigor they deserve.
Introduction
As a physician who trained in internal medicine with a biomedical engineering background, I spent years navigating the intersection of research and patient care. During medical school and my residency training, I learned that the practice of medicine demands rigorous evaluation of evidence—yet I witnessed how easily both patients and providers can be misled by compelling but unsubstantiated health claims. In the end, I left medicine (after completing PGY-1 in a Boston hospital) due to the little impact I thought my interventions were making and the thought that I could help people more elsewhere (like here). I had questions:
- What are the most impactful medical interventions?
- What’s the best bang for your buck (benefit-to-cost ratio)?
- How do you actually implement these interventions in real life
That’s what I hope to show you on this page, which has taken me over 10 years to compile.
Medical training emphasizes systematic diagnosis through evidence hierarchy: starting with the most reliable information sources and working down only when necessary. This same approach applies perfectly to personal health decisions—asking not just “does it work?” but “how well does it work, for whom, and at what cost?”
The stakes are enormous. Americans spend over $50 billion annually on supplements alone (Grandviewresearch), most without evidence of benefit (Harvard Health). Meanwhile, interventions with massive proven benefits—like regular exercise and sleep optimization—remain underutilized. Or where truly dangerous things, like social isolation (social isolation kills more people than smoking 15 cigarettes daily, PubMed, Nature), aren’t talked about enough. Only 5.6% of healthcare interventions have high-quality evidence supporting their benefits (ScienceDirect). This guide bridges that gap by teaching you to think like a physician and scientific researcher about your health choices and, most importantly, improve your life and others’.
Why should you care?
Is what you are taking, doing, or being told to do actually effective? Or nonsense? Is it hurting you, or making you healthier? From the power of sleep and exercise to red wine disasters to “healing” by putting your naked feet on the ground, I’ll try and break through all the noise and show you what actually will help; what beats the placebo (hint: it’s few and far between).
The medical literature contains over 30 million indexed papers, with 4,000 new studies published daily (WHO). Without frameworks for evaluation, consumers inevitably rely on marketing claims, celebrity endorsements, or the latest health trend. Evidence-based health offers a systematic alternative: prioritizing interventions based on strength of evidence and magnitude of benefit (Nih). Here’s what I hope you’ll learn by the end of this (massive) article:
- What is “good” and “bad” evidence?
- What is the measurable impact of evidence-based interventions?
- How to prioritize life changes and interventions?
- What are the highest-impact possible changes for health?
- What are lower-impact changes for health?
- How do you implement this advice in real life?
Warning, Please Read: This is NOT MEDICAL ADVICE—this is educational content mixed with my often incomplete understanding of current evidence. I am a doctor (MD), but I only practiced actual medicine for 1 year as an internal medicine resident, so take everything I say with a generous helping of salt. Do your own research. Make your own decisions. Consult actual healthcare professionals for actual medical stuff.
Also, I tried to minimize jargon and fancy words, but sometimes they’re unavoidable (looking at you, confidence intervals and NNT). If you hit a term that makes your brain glaze over, don’t panic—just pause and look it up. I’ll explain most of them, but I’m neither a statistics professor nor a pharmaceutical executive, so my explanations might be imperfect.
Think of this as a curious person’s attempt to make sense of medical research, not as gospel truth. Your mileage may vary, void where prohibited, and please don’t sue me.
What This Guide Can Do:
- Teach you to think like a physician about health decisions using evidence hierarchies and statistical reasoning
- Prioritize interventions based on effect sizes, cost-effectiveness, and your personal risk factors
- Distinguish between high-impact interventions and marketing noise using quantitative frameworks
- Provide implementation strategies grounded in behavioral science and real-world constraints
What This Guide Cannot Do:
- Replace your doctor: Medical conditions require professional diagnosis and treatment
- Guarantee specific outcomes: Individual variation means results will differ person to person
- Eliminate all health risks: Some factors (genetics, aging, accidents) remain beyond our control
- Make healthy choices easy: Implementation still requires discipline, consistency, and behavior change
Step 1 - Understand "Evidence"
Medical Evidence Hierarchy
Before we dive into what is “good” and “bad” for you, it’s important to understand how these decisions of what is “good” and “bad” are made. Before recommendations are made in the medical community (like “take this pill,” or “exercise a couple times a week”), the recommendations must have research from the top two to three categories of this pyramid. This pyramid is formed and ranked based on the quality of its empirical evidence.
The Foundation: What is Empirical Evidence?
All of these study types rest on a simple but powerful concept: empirical evidence. Empirical evidence means we believe something works because we actually saw it happen—not just because someone said so, “show me, don’t tell me.” Instead of relying on tradition (“my grandmother always said…”), authority (“this famous doctor believes…”), or logical reasoning alone (“this should work because…”), empirical evidence demands direct observation and measurement of what actually happens in the real world.
When we test whether exercise prevents heart attacks, we don’t just theorize about it—we follow thousands of people for years, meticulously tracking their activity levels and health outcomes, then crunch the numbers to see what really happened. This approach has revolutionized medicine over the past century, replacing bloodletting and mercury treatments with interventions that demonstrably save lives.
The evidence pyramid you’re about to see represents different ways of gathering this “show me” evidence, ranked by how well each method eliminates bias, controls for confounding factors, and predicts real-world outcomes.
Without empirical evidence as our foundation, we’d still be making health decisions based on marketing claims, celebrity endorsements, and wishful thinking.
As you begin to do your own research and form your own decisions (which I strongly recommend you do), consider the following pyramid.

The evidence pyramid represents decades of learning about what types of studies actually predict real-world outcomes. For example, if you exercise a certain amount, will you likely live longer? Yes. If you eat a lot of bacon, are you more likely to get colon cancer? Yes.
At the top sit clinical guidelines and meta-analyses, which synthesize multiple high-quality studies. Here’s what they all mean:
- Clinical Practice Guidelines represent synthesized recommendations from expert panels who systematically review available evidence and translate research findings into actionable clinical decisions. The Institute of Medicine (now National Academy of Medicine) established standards for trustworthy guidelines, emphasizing transparency in methodology and management of conflicts of interest (Institute of Medicine, 2011). This is the highest quality material compiled by hundreds of physicians, thousands of studies, and millions of patients’ data.
- Meta-analyses statistically combine results from multiple independent studies addressing the same research question, potentially providing more precise effect estimates than individual trials (thanks mostly to the magic of statistics). When properly conducted with comprehensive searches and appropriate statistical methods, meta-analyses can increase statistical power and resolve conflicting findings across studies. However, their validity depends critically on the quality of included studies and appropriate handling of heterogeneity between study populations and methods (Cochrane Handbook). By combining multiple good studies, you develop information greater than the sum of its parts.
- Randomized Controlled Trials (RCTs) start the pyramid’s second tier. This is the highest grade single “experiment” possible and is used for approving drugs, for example. By randomly assigning participants to treatment (i.e., drug) or control groups (i.e., sugar pills), RCTs eliminate most bias sources that plague observational studies. Double-blind trials, for example, blind the participants and researchers so both have no idea what they are taking (each pill might be labeled “A” or “B,” as opposed to “sugar” or “real drug,” and only a few people have the “key” to what pill “A” and “B” actually are). The GRADE methodology, used internationally to assess evidence quality, starts RCTs with “high quality” designation—they can only be downgraded based on specific limitations (ScienceDirect).
- Observational studies, including cohort studies that follow groups over time, occupy the pyramid’s middle. While valuable for identifying associations and long-term outcomes, they start with a “low quality” evidence designation due to inherent confounding factors because these studies look at people and associations. One famous example is the question of whether red wine is good for you? The problem is, those people who were studied were possibly healthy already and happened to drink a glass of red wine a day. So there were confounding variables (of exercise, diet, social relationships) and only an association between red wine drinking (versus causation). These studies can be upgraded when effects are large, dose-response relationships exist, or plausible confounding would actually diminish rather than create observed effects (ScienceDirect).
- Case series and individual reports form the pyramid’s base. While useful for identifying rare adverse events or documenting unusual responses, they cannot establish causation and often mislead when generalized beyond their specific context. Interesting cases, however, can spur further investigation. For example, the famous story of H. Pylori bacteria and ulcers, where a doctor infected himself to prove the bacteria’s effect; this was a single “case study” that prompted doctors around the world to eventually prove this doctor’s hunch true.
- Animal and laboratory studies provide foundational mechanistic understanding and safety data that inform human research design, but their translatability to human populations remains highly variable. They are at the bottom of the pyramid for a reason. While essential for exploring biological pathways and initial safety assessment, animal models often fail to replicate human physiology, disease progression, and treatment responses. The National Institute of Health emphasizes that fewer than 10% of promising treatments in animal studies successfully translate to human benefit (NIH National Center for Advancing Translational Sciences).
The basis of all of these studies? Statistics.
Why We Need Statistics
(From Sketchplanations.com)
Doing medical research without statistics is like launching a rocket without sensors; you’ll never know if it’s on course until you see an explosion in the sky or it miraculously succeeds. Statistics help us separate genuine medical breakthroughs from expensive placebos, distinguish between “this worked by random chance” and “this worked because of our intervention.”
Here are some essential statistical terms to be aware of:
- P-values tell us how likely it is that we’re seeing results just from dumb luck rather than a real effect. Imagine testing a new headache pill: you give it to 100 people and 80 get better, while in another group of 100 people who got a sugar pill, only 50 got better. The p-value tells you the probability that this 30-person difference happened purely by coincidence—if the p-value is less than 0.05 (meaning less than 5% chance it’s just random), we consider the result “statistically significant.” A low p-value means we can be confident the headache pill is actually working rather than those extra 30 people just happening to feel better by random chance—because nobody wants to take a medication that’s no better than rolling dice (still stuck? this article makes it easy).
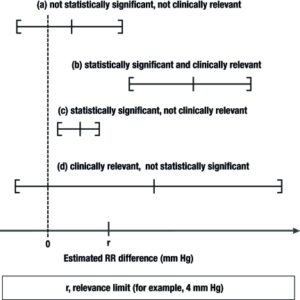
- Confidence intervals provide more meaningful information than p-values alone. Instead of saying “the drug works 23% of the time,” we say “we’re 95% sure the drug works somewhere between 15% and 30% of the time”—it’s like giving yourself wiggle room because we know our measurement isn’t perfect. A 95% confidence interval means we’re 95% confident the true value lies within that range. For example, if a drug reduces heart attack risk by 22.8% (95% CI: 15.2-29.8%), the narrow confidence interval suggests a robust finding unlikely due to chance (Nih1Nih2). If the lower bound of the confidence interval was less than 0%, we wouldn’t be sure if the drug has a benefit or not.
- Number Needed to Treat (NNT) translates research findings into practical terms. How many patients to do you need to give this drug or treatment to save or treat one person? If you have to treat 20 people with a drug for 1 person to benefit, that’s way different from treating 2 people for 1 person to benefit—NNT tells you which treatments are actually worth the hassle. Lower NNTs indicate more effective treatments (Ox). This single metric helps evaluate whether an intervention’s benefits justify its costs and risks (NihScienceDirect).
- Effect sizes measure practical significance beyond statistical significance. This tells you not just “did the treatment work” but “how much did it actually help”—like the difference between a painkiller that reduces your pain from 8/10 to 7/10 versus one that drops it to 2/10. You can quantify this with standard deviation, risk ratios, absolute risk reduction, NNT (like above), and variance. Relative risk (RR) is helpful to know and compares risk between groups—RR of 0.5 means 50% risk reduction.
- Hazard ratios (HR) compare how quickly bad things happen to different groups over time. Imagine tracking 1,000 vaccinated people and 1,000 unvaccinated people for a year: if 2 vaccinated people get severe COVID each month while 10 unvaccinated people get severe COVID each month, the hazard ratio is 2÷10 (amount of people very sick from COVID after vaccinated divided by amount of people very sick from COVID not being vaccinated) = 0.20. This means at any given moment, vaccinated people have only 20% the risk (or 80% lower risk) of getting severely sick from COVID compared to unvaccinated people. Unlike only counting total cases at the end, hazard ratios capture the ongoing, moment-by-moment risk difference throughout the entire study period, which is crucial when people enter studies at different times or some drop out early. Importantly, however, what demographic of people are they looking at? Babies? Elderly? Somewhere in between? This is important when we decide whether or not this evidence applies to us.
- Statistical power is like having enough people in your study to actually see if a drug works. If you’re testing whether a new drug prevents heart attacks, you need thousands of patients—not just 50—because heart attacks are rare and you need to see enough events to know if the drug is really helping. What if those 50 people never have heart attacks? Is your drug magic that stops all heart attacks? Probably not. The FDA typically requires 80-90% power for Phase III trials, meaning the study has at least an 80% chance of detecting the drug’s effect if it’s real. The math depends on how big the effect is (preventing 50% of heart attacks needs fewer patients than preventing 10%), how common the disease is, and how sure you want to be. If a pharmaceutical company tries to get approval with an underpowered study of only 200 patients when they needed 2,000, the FDA will likely reject it because the results could just be random luck rather than proof the drug actually works.
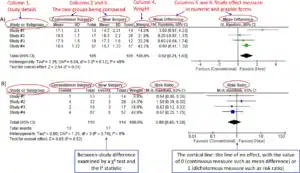
Take a look at the following chart from Dtsch Arztebl Int., it compares the results from 4 studies. The range is the confidence interval, and line is the middle value between the confidence intervals. Importantly, note the “r” on the x-axis, this is the “relevance limit,” or how many mmHg in blood pressure change is relevant. The third bar down, (c), may be confusing. If it’s statistically significant, how can it not be clinically relevant? Well, anything less than a 4 mmHg blood pressure change is clinically irrelevant as decided by some group of researchers and physicians. It’s like a medication decreasing the blood glucose of hyperglycemic diabetic patients 100% of the time by 1mg/dL, sure, it works, but who cares?
So if we have the right level of evidence and the right statistics, we can trust the evidence, right? Let’s do what they say! Well, slow down, we aren’t ready yet. Let’s talk about bias.
Bias
(Image from Sketchplanations)
We’re all walking around with brains that evolved to survive on ancient savannas, not to interpret modern medical research—which creates some fascinating mental shortcuts that can lead us hilariously astray. Take confirmation bias: if you believe vaccines cause autism, you’ll unconsciously notice every story about an autistic child who got vaccinated while completely ignoring the millions of vaccinated kids who are perfectly fine. Or consider the availability heuristic, where we judge risks based on how easily we can remember examples—people often fear plane crashes more than car accidents because plane crashes get wall-to-wall news coverage, even though you’re statistically more likely to die driving to the airport than flying to your destination.
These same cognitive biases don’t magically disappear when scientists put on lab coats—they just get more sophisticated and potentially more dangerous. The famous case of Vioxx, a painkiller that increased heart attack risk, shows how bias can be deadly when researchers and the company highlighted studies showing benefits while downplaying cardiovascular risks (the drug was pulled from the market after causing thousands of heart attacks).
Understanding these biases helps you spot when research might be telling you a story that’s too good (or bad) to be true, whether it’s coming from a supplement company or a prestigious medical journal.
- Publication bias happens because journals love publishing exciting “this drug works!” studies but hate boring “this drug does nothing” studies—for every one plane crash there are millions of safe flights, but how often do you see news headlines about safe flights? Older antidepressant research shows this perfectly: only 51% of actual trials showed the drugs worked, but if you only read published studies, you’d think they worked way more often because the negative studies got buried in filing cabinets instead of medical journals (antidepressants are beneficial, but selective publishing set the medical community back).
- Selection bias occurs when your study participants don’t actually represent the people who would use the treatment in real life—like testing a new arthritis drug only on marathon runners and then claiming it works for all elderly people. An elderly fitness study conducted at a swimming pool automatically excludes elderly people who can’t swim or stay active, making the results useless for predicting how the average couch-bound grandparent would respond to the same intervention (PubMed).
- Confirmation bias is when researchers unconsciously cherry-pick data that supports what they already believe, like a sports fan who only notices when their “lucky” jersey helps their team win but ignores all the losses. Researchers who think a supplement works might stop collecting data the moment results look good, ignore patients who got worse, or design unfair comparisons that stack the deck in favor of their pet theory. I am trying (and likely failing) to avoid confirmation bias when writing this massive article, as I believe in evidence-based advice and the benefits of it, which leads me to look for articles and research that support my views. I also feel a certain way about most supplements…
- P-hacking is like buying 20 lottery tickets and then bragging that you’re a “winner” because one of them paid off—if you test enough different health outcomes, you’ll find one statistically significant result purely by chance (p < 0.05), but reporting only that one “significant” finding without mentioning the 19 failures is deeply misleading. This turns scientific research into a fishing expedition where researchers keep casting their nets until they catch something impressive-looking to publish (Statistics By Jim, NCBI).
This is why the evidence pyramid is so important, and the quality of evidence decreases dramatically as you drop below controlled trials.
A Personal (Opinionated) Note on Correlation, Association, and Causation:
Before we dive deeper, I want to break from the rest of this more objective guide and give you a brief personal opinion that’s informed by my own experience reading thousands of studies—and being misled by many.
Here’s the uncomfortable truth: I don’t really trust most studies. Not because science is broken, but because I’ve seen how even good science can be misused, misunderstood, or manipulated. Especially when it comes to association and correlation—two terms that sound rigorous but often tell us little about what actually causes an outcome.
If a study says “people who drink coffee have lower rates of Alzheimer’s,” that’s association. It doesn’t mean coffee prevents Alzheimer’s. Maybe coffee drinkers also tend to be more educated, sleep better, or exercise more—all of which affect brain health. Unless we randomize who drinks coffee and who doesn’t—and control for every confounder—we have no idea if the coffee is actually doing anything.
And here’s where things get messy: even prospective studies, which are supposedly stronger than retrospective ones, can fall victim to statistical sleight-of-hand. Ever heard of p-hacking? It’s when researchers test 20 different outcomes (maybe cholesterol, mood, weight, skin glow, shoe size…) and then only publish the one that “worked.” Voilà! A magic supplement. This isn’t rare—it’s shockingly common.
That’s why, for my money, randomized controlled trials (RCTs) are the gold standard. If it’s not an RCT, I treat it like an interesting hypothesis—not a conclusion. And even RCTs can be flawed, underpowered, or biased (as we’ve just learned). But at least they try to isolate cause from noise.
Finally, beware the seductive certainty of mechanisms. You’ll see scientists say things like, “This works because it increases brain-derived neurotrophic factor” or “This targets X pathway.” But we’ve been wrong before. Lobotomies were once based on a mechanistic model of calming brain circuits. Hormone replacement therapy was supposed to “fix” aging because a decrease in hormones (like estrogen) was thought to “cause” aging. In medicine, our understanding of why something works often lags decades (or centuries) behind an understanding of the mechanism of action (how the drug actually works), and even then, we’ve been wrong.
So here’s my suggestion: don’t just believe what I write here. When I link to studies, check them. Are they RCTs? Are they meta-analyses of high-quality trials? Or are they correlations dressed up as causation? This distinction is everything.
Let’s not fall for impressive-sounding claims without understanding what they’re built on. If we’re going to build a healthier life, we should build it on solid ground.
Ok, but scientists all know this right? That’s why they get to wear the fancy white coats and we call them “doctors.” Critical mistakes don’t happen in real life right?
Examples of Evidence Gone Wrong
Sometimes the scientific process works exactly as it should—initial evidence points one way, better evidence comes along and corrects course, and we end up with treatments that actually help people. But sometimes it takes decades, thousands of unnecessary deaths, or entire populations following harmful advice before we realize we got it spectacularly wrong. These cautionary tales aren’t meant to make you distrust all medical research, but rather to show why the quality of evidence matters so much and why “we’ve always done it this way” isn’t a good enough reason to keep doing something.
- Hormone Replacement Therapy (HRT) illustrates how observational evidence can mislead (hmm, where was that on the pyramid again?). Throughout the 1990s, observational studies suggested HRT reduced heart disease risk, leading to widespread prescribing for disease prevention. However, the 2002 Women’s Health Initiative randomized controlled trial revealed increased risks of breast cancer, stroke, and blood clots (the pyramid strikes again!). This reversal occurred because observational studies suffered from confounding—healthier, more educated women were more likely to use HRT and have better cardiovascular outcomes independent of hormone use.
- Dietary fat recommendations demonstrate the dangers of building guidelines on weak evidence. 1970s-1980s dietary guidelines recommended reducing saturated fat based primarily on observational studies like the Seven Countries Study. These recommendations led to increased carbohydrate consumption and contributed to rising obesity rates. Subsequent RCTs, including the Women’s Health Initiative, showed no benefit from low-fat diets, while Mediterranean diet studies demonstrated benefits of certain fats (JACC, Nih)
- Vioxx withdrawal shows how post-marketing surveillance can reveal risks missed in initial studies. Approved in 1999 based on gastrointestinal safety data, cardiovascular risks emerged only after the VIGOR study in 2000 and were confirmed by the APPROVe trial in 2004, leading to voluntary withdrawal (remember p-hacking?). This timeline reinforced the importance of long-term safety data and comprehensive risk assessment (Fda).
- Red wine gone wrong. The famous French Paradox and Copenhagen Heart Study suggested red wine drinkers had dramatically lower heart disease risk, leading to a 40% surge in U.S. wine consumption after the 1991 60 Minutes broadcast. But researchers acknowledged that “wine-consuming individuals might have better access to medical care and also might have a better management of cardiovascular risk factors” because “red wine is usually more expensive than other beverages” The wine drinkers weren’t just drinking differently—they were wealthier, more educated, and had better healthcare access overall. Meanwhile, to get the protective dose of resveratrol from the studies, you’d need to drink 500-2,700 liters daily. It was never the wine—it was the privileged lifestyle of people who could afford expensive wine (OUP). The lifestyle difference involved many confounding variables (a confounding variable is when something else is the real reason two things seem connected, like how ice cream sales and drowning both go up in summer, but it’s not the ice cream causing drowning, it’s the hot weather making people both buy ice cream AND go swimming more).
These examples aren’t meant to scare you away from medical research—they’re reminders that science is a self-correcting process, messy and imperfect, but ultimately pointing us toward better treatments over time. The key lesson isn’t “don’t trust any studies” but rather “demand good evidence before making major health decisions.” When someone tells you to take a supplement, follow a diet, or avoid a medication, ask yourself: what quality of evidence supports this claim, who conducted the research, and what biases might be lurking beneath the surface?
And, remember, in the end the goal of all this research is to (hopefully) help people: vaccines have extended global life expectancy by 10-20 years saving about six lives a minute, the Framingham heart study resulted in an ~82% drop in cardiovascular mortality in working-age men, cataract surgery has granted vision to 100+ million people worldwide, hip and knee replacements have allowed millions to walk again, and the list goes on.
However, when we have rock-solid evidence that something works, we’re still left with a crucial question: is it worth it for me? A treatment might reduce your risk of heart disease by 20% in a randomized controlled trial, but if your baseline risk was already tiny (say 1%), that impressive-sounding percentage might translate to almost no real benefit (0.2%). And what if everyone who takes this drug has a 10% risk of going blind? Would you take that drug?
Therefore, next we will talk about marginal impact. Understanding marginal impact—the actual difference a treatment will make in your specific situation—is where the rubber meets the road in evidence-based decision making.
Step 2 - Understand "Marginal Impact"
Imagine two friends: one spends $100 monthly on supplements that might extend their life by a few days, while the other spends that same $100 on a gym membership and gains 2-4 years of life. Same money, wildly different returns on investment. This is marginal impact in action—the art of distinguishing between interventions that actually move the needle versus those that just move money from your wallet to someone else’s.
The concept of marginal impact separates interventions that meaningfully improve health outcomes from those that provide minimal benefit despite substantial cost or effort.
What’s the (quantifiable) difference?
Let’s look at some examples of just how relevant this is.
- Exercise (yay!) represents the gold standard for high-marginal-impact interventions—think of it as the Swiss Army knife of health improvements. Meta-analyses show physically active individuals experience 22-35% lower all-cause mortality compared to sedentary individuals (Biomedcentral, PubMed), which translates to actually living 0.4 to 4.2 years longer (NCBI). The dose-response relationship shows remarkable consistency: just seven hours weekly of moderate activity provides 24% mortality reduction versus no activity ScienceDirect, OUP Academic), while resistance training for only 60 minutes weekly provides 27% mortality reduction (HR=0.74, 95% CI: 0.64-0.86) (ScienceDirect, PubMed). These effect sizes absolutely dwarf most pharmaceutical interventions—it’s like having a miracle drug that’s free and has only positive side effects. I
- Supplements (nay) on the other hand… General vitamin supplementation is incredibly expensive for the tiny health benefit it provides—costing over £600,000 to add one healthy year to someone’s life (Nice). Most weight-loss supplements show modest 2-pound average weight loss versus placebo in short-term studies, with no evidence of sustained benefits or mortality reduction (EatingWell). Some supplements—notably vitamin D for those who are deficient—do show moderate benefits, such as a statistically significant 16% reduction in cancer mortality in one large meta-analysis, but even this pales in comparison to the well‑documented life‑lengthening and disease‑preventing effects of regular exercise, high‑quality sleep, and a balanced diet. Not to mention that the vast majority of supplements have no evidence whatsoever.
- Sleep optimization (yay!) provides another high-impact example with quantifiable benefits. Studies consistently show U-shaped mortality curves with 7-hour sleep duration providing optimal outcomes. Short sleep (<7 hours) increases mortality risk by 12% (RR: 1.12, 95% CI: 1.06-1.18), while long sleep (>7 hours) increases risk by 30% (RR: 1.30, 95% CI: 1.22-1.38) (Ahajournals, Nature) Population-level analyses suggest inappropriate sleep duration contributes to over 1 million cardiovascular events annually in the United States (Frontiers).
- Plastic straw bans (nay). Can we apply this impact-based approach more broadly? Yes! Let’s talk plastic straws. Reducing plastic pollution is genuinely important—microplastics harm marine life, disrupt food chains, and potentially affect human health through bioaccumulation. But plastic straws represent only 0.025% of the 8 million tons of annual ocean plastic pollution, making their elimination virtually meaningless for ocean health. Hong Kong’s experience perfectly illustrates this disconnect—despite achieving a 40% reduction in straw consumption (from 1.7 billion to 1 billion straws) between 2017-2020, overall plastic waste increased 10.3% during the same period. This type of symbolic environmentalism diverts attention and resources from interventions that actually have massive environmental impact. The problem? Incentives. The low-hanging fruit of plastic straws allows companies and social media personalities to garner attention and have a moral “get out of jail” card. What about industrial waste, abandoned fishing nets (which comprise 46% of ocean plastic), improved waste management systems in developing countries, or reducing single-use packaging from major corporations? These unglamorous interventions would actually move the needle on ocean health and ecosystem preservation. Instead, we get feel-good policies that let politicians claim environmental victories while the real problems persist. This principle applies equally to health interventions: symbolic gestures that make us feel virtuous often crowd out the unglamorous but high-impact activities that actually move the needle on population health outcomes.
- Antibiotics (yay?) While antibiotics can be life-saving for serious bacterial infections like pneumonia, robust meta-analyses and randomized controlled trials consistently show that for many common bacterial infections, antibiotics reduce symptom duration by only 1-2 days on average. For acute otitis media (ear infections), a landmark individual patient data meta-analysis examining 1,642 children showed only a 14% absolute improvement in clinical outcomes overall, while 60% of placebo-treated children were pain-free within 24 hours, demonstrating the self-limiting nature of most ear infections. Similarly, for acute bronchitis, the most recent Cochrane Review analyzing 17 trials with 5,099 participants found antibiotics reduced days feeling ill by only 0.64 days and days with impaired activity by 0.49 days. The research consistently shows that adverse effects from antibiotics occur in 1 out of every 10-25 patients treated, while benefits occur in only 1 out of every 7-20 patients.
*SIDE NOTE*: Incentives: If exercise is more beneficial than 90% of drugs, why isn’t it advertised everywhere? This is why it’s so important to do your own research. Where is the incentive for anyone to advertise exercise? Maybe the government and certain health insurance companies, but the incentive is much greater (at least in the USA) for pharmaceutical companies to sell drugs and for hospitals to provide interventional treatments and surgeries (I’m looking at you RVU). Consider the tobacco industry’s decades-long campaign promoting cigarettes as healthy—doctors literally appeared in advertisements claiming “More doctors smoke Camels than any other cigarette” throughout the 1940s and 1950s, even as internal company documents revealed they knew about cancer risks (Stanford Research into the Impact of Tobacco Advertising). The industry spent billions creating doubt about scientific evidence while promoting their products as beneficial for digestion, weight control, and even throat health. Why? Money money moneyyyy.
Charlie Munger frequently highlighted how incentives drive behavior, noting that “the power of incentives to cause rationalized and often terrible behavior is enormous.” A pharmaceutical company can spend $1 billion (and often does) developing and marketing a diabetes drug that patients take daily, but no one profits from telling people to walk 30 minutes daily—despite exercise often being more effective for blood sugar control than many medications. Again, I don’t think pharmaceutical companies are inherently evil or contain more bad actors than any other large organization, but it’s crucial to understand where the incentives lie when evaluating health advice. Follow the money, question the source, and remember that the most advertised solution isn’t always the most effective one for your health.
Does this apply to me?
Understanding whether research findings apply to your specific situation requires careful examination of study populations and your personal risk profile. This concept, called “external validity” or “generalizability,” determines whether impressive-sounding study results actually translate to meaningful benefits for you personally.
Age and Demographic Considerations:
- “Resveratrol is the fountain of youth!… if you’re a lab mouse” The famous 2006 study showed resveratrol extended mouse lifespan by up to 30%, leading to massive supplement sales. But follow-up studies found issues and it never translated to humans (The Lancet, Uclahealth). In humans, you’d need to drink 500-1000 bottles of red wine daily to get the mouse-effective dose. The resveratrol supplement industry is built on mouse studies that have never translated to humans.
Baseline Risk Assessment:
Age and Baseline Risk Assessment:
- “Calcium supplements build strong bones!… but if you’re over 50 it does nothing and might increase your risk for a heart attack.” Studies show calcium supplementation can significantly boost bone density, but the benefits are highly age-dependent. Research found that “calcium supplementation produced larger effects in individuals between the ages of 20 and 35 than in people younger than 20” and “increasing calcium intake in older people is unlikely to translate into clinically meaningful reductions in fractures”. For young adults still building peak bone mass, extra calcium provides real structural benefits. But for healthy 50-year-olds who’ve already reached peak bone density, calcium supplements show little benefit and may even increase cardiovascular risks. The window for bone-building closes after age 35—you can’t make up for lost time with pills (elifesciences).
Genetic and Individual Variation:
- “Smoking helps you be healthier!… if you are at risk for ulcerative colitis… and don’t mind dying from lung cancer” Multiple studies show that smoking paradoxically protects against ulcerative colitis, with current smokers having a 42% reduced risk compared to never-smokers (OR: 0.58, 95% CI: 0.45-0.75) But this is a rare exception where one disease benefit is massively outweighed by cancer, heart disease, and lung damage risks. My guess is that there is some confounder in these studies that we are missing.
Comorbidity and Medication Interactions:
- “High-intensity exercise prevents heart attacks!… unless you have underlying heart disease.” The Copenhagen City Heart Study found that more jogging wasn’t necessarily better and could be harmful. Those with underlying heart conditions face a 17-fold higher cardiac event risk during intense exercise.
What’s the cost?
Every health intervention involves tradeoffs—money, time, effort, and potential risks that must be weighed against anticipated benefits. Smart decision-making requires honest assessment of these full costs, not just the advertised benefits.
Imagine you are a neurosurgeon deciding whether or not to do surgery on a patient with brain cancer. You are likely weighing a couple of things: will the surgery extend the patient’s life? And for how long? What about the quality of life? What are the risks of the surgery? What’s the chance the patient dies from this surgery? If the surgery has a 10% chance of adding 5 years to the patient’s life, but a 50% risk of the patient dying on the table, what would be your recommendation? Nearly all medical decisions come with a cost. The “easiest” decisions are when the benefits dramatically outweigh the costs.
- Money extends beyond obvious expenses to include opportunity costs and hidden fees. A gym membership costs $50 monthly, but also requires transportation, workout clothes, and potentially childcare—easily doubling the real expense. Prescription medications often involve not just copays but also monitoring costs (regular blood tests), potential side effect treatments, and lost productivity from medical appointments. The UK’s cost-effectiveness analysis revealed that exercise programs achieve remarkable value at €4,577-€86,877 per QALY, while universal vitamin supplementation costs £620,898 per QALY—making exercise roughly 100 times more cost-effective than general supplementation (Bjgp, Nih, Nice).
Side Note, What’s a “QALY?”: One QALY equals one year of life in perfect health (Quality of Life Year). If a treatment extends life by two years, but the person lives those years at 50% health quality (e.g., with pain or disability), it provides one QALY. This metric allows researchers and policymakers to compare the cost-effectiveness of different health interventions—whether it’s a $4 blood pressure pill or a $100,000 cancer drug. For example, a treatment that costs $50,000 and adds 1 QALY is often considered cost-effective in the U.S. healthcare system. QALYs are widely used by organizations like NICE in the UK and the Institute for Clinical and Economic Review (ICER) in the U.S. to guide funding decisions (NIH, NICE, ICER). While the model isn’t perfect (e.g., it can undervalue treatments for people with chronic disabilities), it remains one of the most widely accepted tools for comparing the real-world impact of different health strategies.
This chart below shows how a treatment can improve both how long someone lives and how well they feel during that time. The vertical axis (left side) shows “health-related quality of life,” where 1.0 means perfect health and 0.0 means death, while the horizontal axis shows time in years. Person A (blue area) didn’t get the treatment and had lower quality of life and died earlier, while Person B (blue + tan area) got the treatment, lived longer, and had a better quality of life—so they gained more QALYs (quality-adjusted life years), which is how we measure both time and health in one number. I’d want the treatment that B got!

Side note: Incentives for the American Healthcare System: The numbers are staggering when you apply health economics rigor. Exercise interventions cost $4,648-$19,788 per Quality-Adjusted Life Year (QALY), while most pharmaceutical interventions exceed $100,000 per QALY (I-jmrPubMed). Sleep optimization is essentially free yet provides benefits that would cost $50,000-$150,000 per QALY if delivered through medical intervention.
The healthcare system’s incentives become crystal clear through this lens, and they might not be for the best. Fee-for-service models reward procedures over prevention, creating a system where healthcare systems profit from more procedures than prevention (PrognoCIS EHR, Commonwealthfund). A sleep optimization program generates no billable procedures, despite preventing more deaths than the most expensive medical interventions. Again, I don’t believe it’s the medical system’s fault, and America has some of the most advanced healthcare technology in the world. It is simply important to note where the incentive is. If the hospital doesn’t make money, it can’t pay doctors and workers, keep the lights on, and treat patients. What is the solution? I’m not sure. More insurance incentives for prevention? But how do you track that? What’s the reimbursement model? Who pays?
- Time cost represents the scarcest resource for most people. The minimum effective dose of exercise (60 minutes weekly resistance training + 150 minutes weekly moderate cardio) requires approximately 3.5 hours weekly—manageable for most people. However, elaborate supplement regimens, complex dietary protocols, or multiple medical appointments can consume far more time while providing inferior health returns. Not to mention even more time-consuming things like coffee enemas, peyote microdosing ceremonies, or standing on your head for 45 minutes while chanting mantras to optimize your chakra alignment, which provide no benefit and may even cause harm.
- Side effects and safety risks vary dramatically between interventions. Exercise carries minimal serious risk for most people—primarily musculoskeletal injury risk of approximately 1-5 injuries per 1000 hours of activity, usually minor and temporary. In contrast, pharmaceutical interventions often involve significant side effect profiles. Statins cause muscle pain in 10-15% of users and rare but serious liver toxicity. Nonsteroidal anti-inflammatory drugs (NSAIDs) increase cardiovascular risk by 20-50% and cause thousands of serious gastrointestinal bleeds annually. Even “natural” supplements aren’t risk-free—high-dose vitamin E increases bleeding risk, while herbal supplements can interact dangerously with prescription medications. And when many of these supplements do virtually nothing, the cost outweighs the benefit.
- Psychological and social costs come into play. Obsessive calorie counting or supplement regimens can develop into unhealthy relationships with food and health. Extreme dietary restrictions may interfere with social eating situations and family relationships. Being forced to stay in the hospital for a couple of months can make patients more depressed.
- Opportunity costs represent perhaps the most overlooked expense—resources spent on one intervention can’t be used for alternatives. Money spent on unproven supplements could fund gym memberships, healthier food, or preventive medical care. Time spent researching and implementing complex supplement protocols could be used for meal preparation, exercise, or stress management. The key question isn’t whether an intervention has any benefit, but whether it provides better returns than available alternatives given your specific circumstances and resources. This is the most difficult, yet most impactful cost to understand.
Understanding marginal impact means you can now cut through health marketing noise by asking the right questions: What’s the actual effect size? What’s the Number Needed to Treat? How does this compare to proven alternatives? The evidence reveals stark differences across all types of interventions.
Exercise provides 22-35% mortality reduction (HR: 0.65-0.78) with cost-effectiveness of €4,577-€86,877 per QALY, while general supplementation costs £620,898 per QALY for minimal benefit. Vaccines demonstrate exceptional value with 95% relative risk reduction for COVID-19 and cost-effectiveness ratios consistently below $100,000 per QALY. In contrast, many surgical interventions—while potentially life-saving—carry significant tradeoffs: that fictional neurosurgery example with 10% chance of adding 5 years but 50% risk of operative mortality illustrates the importance of weighing costs and benefits.
When you evaluate interventions using confidence intervals, absolute risk reduction, and Number Needed to Treat instead of marketing claims or emotional appeals, clear hierarchies emerge. You now have the tools to distinguish between interventions that meaningfully extend healthy lifespan (lifestyle modifications, preventive care, targeted medications) and those that don’t. The question isn’t whether an intervention has any benefit—it’s whether it provides better returns than proven alternatives given your finite resources and personal risk profile.
Doing this properly is like putting your money in an index fund versus day trading stocks. Where do the majority of people see the greatest gains over time, controlling for nearly all other variables?
Step 3 - Understand Prioritization
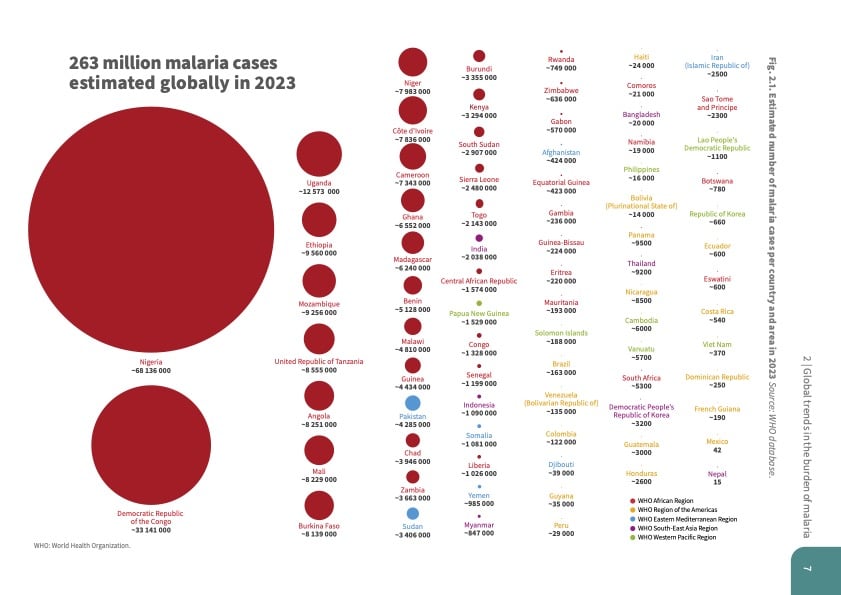
Imagine two people: Sarah, a 35-year-old software engineer in San Francisco spending $200 monthly on adaptogens and biohacking gadgets, and Amara, a 35-year-old teacher in rural Malawi choosing between a $2 mosquito net and her family’s dinner. Sarah’s biggest health threat is sitting 10 hours daily and chronic stress. Amara’s biggest threat is malaria, which kills over 579,000 people annually in sub-Saharan Africa (WHO). Same age, same planet, completely different health priorities.
This isn’t just about geography—it’s about understanding that health prioritization depends entirely on your specific threats, resources, and life stage. A Roman soldier in 50 AD worried about battlefield infections and traumatic injuries, not heart disease or diabetes. An 18th-century European feared smallpox and cholera, which killed 30% of children before the age of 5 (Our World in Data). Today’s health landscape would be unrecognizable to our ancestors, just as our descendants might view our current obsessions with cold plunges, supplements, and coffee.
A great example of “what’s relevant to me” is statin therapy: the NNT for all-cause mortality in primary prevention is 138 patients treated for 5 years to prevent one death (NCBI, Gpevidence) However, who are those 138 patients? For a 40-year-old marathon runner with perfect lipids, this intervention approaches medical malpractice. For a 65-year-old diabetic with multiple cardiovascular risk factors, it’s potentially life-saving. The intervention hasn’t changed—the baseline risk has, fundamentally altering the cost-benefit calculation.
This is why one-size-fits-all health advice is subpar. Your optimal intervention portfolio depends on your current health status, age, genetics, and risk factors. The evidence-based approach requires building decision trees that account for these variables, not following generic recommendations designed for statistical averages.
So, how do you prioritize interventions for you?
Geography
Your physical location determines which diseases threaten you most, what medical care you can access, and which environmental hazards require attention—making geography one of the strongest predictors of health outcomes. Take a look at the two graphs from the WHO that show cause of death from low-income versus high-income countries in 2021. Note the differences in malaria, heart disease, lower respiratory infections, and Alzheimer’s.
Low-Income

High-Income

In the U.S., heart disease kills ~695,000 people annually (CDC); in the DRC, malaria causes ~12% of all deaths and ongoing conflict has displaced over 5.7 million people (WHO); while in Scandinavia, low infectious disease rates shift the burden to dementia (the leading cause of death in Sweden) and suicide, especially in rural and northern areas (OECD). The highest impact health interventions are wildly different depending on whether you are in the USA, the DRC, or Scandinavia. Here’s how geography comes into play:
- Access to healthcare: Rural areas suffer from a 25% shortage of primary care physicians (39.8 per 100,000 vs 53.3 in urban areas) and force residents to travel 7.2 miles on average to reach healthcare versus 1.1 miles for urban dwellers in the USA. These access disparities translate directly into health outcomes: Appalachian regions show 16% higher infant mortality rates and 444.4 deaths per 100,000 compared to 332.3 in non-Appalachian areas. Expanding worldwide, cesarean section rates range from 1.1% in Chad to 62.9% in the Dominican Republic, far outside the WHO-recommended 10-15% range. Sub-Saharan Africa achieves only 5% C-section access while Latin America/Caribbean reaches 43%. A woman’s lifetime risk of dying from pregnancy-related causes is 1 in 5400 in high-income countries but rises to 1 in 37 in sub-Saharan Africa, where maternal and neonatal mortality rates remain highest due to limited access to emergency obstetric care (WHO). So your chances of dying from childbirth can change by 100x depending on where you are.
- Disease burden: Malaria exemplifies geographic disease concentration—94% of the world’s 263 million cases and 95% of 597,000 deaths occur in the WHO African Region, with just four countries accounting for over half of all deaths. The $2 mosquito net that saves lives in Malawi would be useless for someone in Iceland. Air pollution mortality shows similar geographic concentration: Black Americans face the highest PM2.5 exposure at 9.38 μg/m³ and roughly 350 deaths per 100,000 people, compared to less than 100 deaths per 100,000 for other racial groups. If you live in polluted urban areas, air filtration and location choices become high-priority health interventions. If you live in certain parts of Africa, you want a mosquito net. If you live in certain parts of Greenland, you want a psychiatrist.
- Climate threats: Heat-related deaths among those over 65 increased by 85% between 2000-2004 and 2017-2021, while the WHO projects 250,000 additional yearly climate-related deaths by the 2030s. However, cold-related mortality actually exceeds heat-related deaths by 5.37 times globally, with rates reaching 96.37 per 100,000 in Uzbekistan and 91.58 per 100,000 in Lesotho. Climate prioritization depends entirely on your location: someone in Phoenix needs heat adaptation strategies, while someone in Minnesota requires cold protection and vitamin D supplementation due to limited sun exposure (especially >40° latitude from October-March). Climate change creates radically different survival stakes depending on where you live: a wealthy homeowner in Norway may barely notice rising temperatures, while a farmer in Bangladesh faces mortal danger regularly from intensified flooding, saltwater intrusion, and crop failure that threaten both livelihood and life (IPCC).
- Sanitation and water access: Basic sanitation remains one of the most geographically unequal determinants of health. Over 2 billion people globally drink water contaminated with feces, leading to 485,000 childdeaths annually from diarrheal disease—primarily in South Asia and Sub-Saharan Africa (WHO). In countries like Chad and the Central African Republic, less than 25% of the population has access to safely managed drinking water, compared to nearly 100% in countries like Switzerland or Japan. For people in these regions, clean water access is not a wellness upgrade—it’s the difference between life and death, especially for children under 5. Below is a graph from the WHO showing the mortality rate per 100,000 people due to water, sanitation, and hygiene (WASH). Chad and Lesotho have nearly 100 times the rate of places like Australia and Switzerland.

- Vaccination coverage: Where you’re born determines whether you’re protected against deadly but preventable diseases. In low-income countries, only 70% of children receive the full DTP3 vaccine series (diphtheria, tetanus, and pertussis), compared to over 95% in most high-income nations (WHO). This gap fuels the resurgence of diseases like measles, which caused over 136,000 deaths globally in 2022, especially in countries like Nigeria, Pakistan, and the DRC. Meanwhile, a child in France may face more risk from vaccine misinformation than from the diseases themselves. Vaccine equity isn’t just a global goal—it’s a geographic determinant of survival.
Putting it all together, here’s a couple of charts on life expectancy, homicides, malaria, obesity, maternal mortality, and pollution by country from the WHO:





Side Note, Blue Zones: So, can you move somewhere and instantly increase your life expectancy? Maybe. The so-called “Blue Zones”—regions like Okinawa (Japan), Sardinia (Italy), and Nicoya (Costa Rica)—are geographic pockets with the world’s highest concentrations of people living past 100. Despite cultural differences, these regions share striking lifestyle commonalities: plant-predominant diets, regular physical activity built into daily life, low alcohol and sugar intake, strong social ties, and natural environments that encourage movement and connection. However, top longevity researchers caution against over-romanticizing these regions: most Blue Zone data is observational, vulnerable to survivor bias, and rarely adjusted for selective out-migration, poor vital records, or socioeconomic confounders—meaning their principles are useful, but their life expectancy claims should be interpreted carefully.
Demographics
Social and economic factors create the largest health disparities in developed nations, with age, income, and weight status serving as powerful predictors of disease risk and life expectancy.
In the U.S., the richest men live 15 years longer than the poorest (JAMA), while people with severe obesity (BMI ≥ 40) lose up to 9.1 years of life (JAMA). But how you’re likely to die also shifts with age: for those aged 15–29, the leading causes are accidents (19%), suicide (17%), and homicide (12%), whereas after age 50, heart disease and cancer dominate, accounting for over 50% of all deaths (CDC FastStats).
- Income: Money literally buys years of life through multiple pathways: better food access, safer neighborhoods, reduced stress, superior healthcare access, and time for self-care. If you’re in the bottom income quintile, addressing financial stability through career development, education, or location changes provides massive health returns that dwarf most medical interventions.
- Age: In the USA, the steepest mortality increases occur in middle age, with death rates jumping from 163.4 per 100,000 at ages 25-34 to 453.3 per 100,000 at ages 45-54. Age determines which threats matter most: for people aged 15-29, accidents (particularly motor vehicle crashes) represent 19% of deaths, followed by suicide (17%) and homicide (12%). Ages 30-49 shift toward early chronic disease prevention, with cancer becoming the leading cause of death (25%), followed by heart disease (22%). Ages 50+ require focus on chronic disease management, with heart disease dominating (30% of deaths). This is highly geography dependent of course, in Mexico homicide is the leading killer between the ages of 15-44, while in sub-Saharan Africa it’s infectious diseases and violence (WHO).
- Weight: Meta-analysis of 82 studies involving 2.7 million patients reveals a U-shaped mortality curve with the lowest risk at BMI 25-30 kg/m². Counterintuitively, mild overweight shows protective effects (HR 0.94, 95% CI: 0.90-0.97), while severe obesity dramatically increases risk—Class III obesity (BMI 40-49.9) carries a hazard ratio of 2.51 (95% CI: 2.30-2.73) for women. Young adults experience greater years of life lost from obesity-related diseases—Black males aged 40-49 can lose up to 11.7 years from obesity-related conditions. Severe obesity reduces life expectancy by 9.1 years for men and 7.7 years for women. Being severely overweight affects nearly every health outcome: increased surgical complications, reduced cancer survival, higher infection rates, and accelerated aging. If your BMI exceeds 35, weight management provides pharmaceutical-grade mortality benefits that exceed most other interventions.
- Education: Education is one of the strongest predictors of long-term health: U.S. adults without a high school diploma die 8–10 years earlier on average than college graduates, even after adjusting for income and race (Case & Deaton, Brookings, 2021). Lower educational attainment is linked to higher rates of smoking, obesity, and delayed medical care, while higher education improves health literacy, preventive care use, and job access. Globally, increasing educational attainment—particularly for women—has been linked to lower child mortality, improved vaccination rates, and better maternal health outcomes, making it one of the most cost-effective public health strategies (UNESCO).
- Gender: Gender profoundly shapes health outcomes: globally, women live 5–7 years longer than men but experience more years of disability and chronic pain, while men die earlier from cardiovascular disease, violence, and substance abuse (GBD 2019; WHO, 2023). In the U.S., men account for nearly 80% of suicide deaths, while women are twice as likely to suffer from depression. Worldwide, gender inequality in healthcare access, education, and employment exposes women in low-income countries to greater risks of maternal death, violence, and undernutrition, while cultural norms also prevent many men from seeking mental or preventive care (Lancet Commission on Gender and Global Health). The infographic below from the CDC shows that males in the USA are more prone to death from things like heart disease and cancer than females.

Genetics, Medical Conditions, and Social Connections
Individual risk factors—from inherited genes to acquired diseases to social relationships—create predictable health outcomes that can guide intervention prioritization with remarkable precision.
Genetic predisposition alone places 1 in 5 people at high risk for major diseases like heart disease and diabetes (eMERGE Network), while individuals with 10+ chronic conditions lose up to 17.6 years of life compared to healthy peers (CMS, 2023). And being socially isolated? It raises your risk of early death by 33%, an effect size on par with smoking or obesity (PLOS Medicine).
- Genetics and family history: The eMERGE Network’s clinical implementation of polygenic risk scores across 25,000 diverse participants found that 20.6% of individuals had high genetic risk for at least one major condition. High-risk individuals (top 2.5%) face 2-3x increased risk for coronary heart disease (OR: 2.0-3.0), while those in the top 2% for diabetes risk show 2-4x increased risk. Family history quantifies inherited risk across multiple diseases: premature parental cardiovascular disease increases risk by 75% for paternal history and 60% for maternal history, while sibling CVD increases risk by approximately 40%. First-degree relatives with breast cancer nearly double an individual’s risk. If your parents died young from preventable diseases, those diseases become your highest-priority prevention targets.
- Chronic diseases: Medicare data from 2023 reveals that individuals with no chronic conditions at age 67 can expect 22.6 additional years of life, while those with 5 conditions lose 7.7 years (14.9 years remaining) and those with 10 or more conditions lose 17.6 years (5.0 years remaining). Each additional chronic condition reduces life expectancy by an average of 1.8 years (range: 0.4-2.6 years). Modern chronic disease management provides substantial life expectancy gains: the SPRINT trial demonstrated that intensive blood pressure control (target <120 mmHg systolic) reduces major cardiovascular events by 27% and all-cause mortality by 27% (HR = 0.73, 95% CI: 0.60-0.90). If you have poorly managed diabetes, hypertension, or heart disease, optimizing these conditions provides years of life gained that completely dwarf trendy health interventions.
- Social connections: Meta-analysis of 36 studies involving 1.3 million participants shows social isolation increases mortality risk by 33% (HR = 1.33, 95% CI: 1.26-1.41). Strong social relationships provide a 50% increased likelihood of survival (OR = 1.50, 95% CI: 1.42-1.59)—an effect comparable to smoking cessation or obesity reduction. Marriage provides protective effects (HR = 0.72, 95% CI: 0.56-0.93) compared to never being married. Social isolation kills with effect sizes that rival major medical conditions. If you’re socially isolated, building relationships and community connections provides measurable mortality benefits that exceed most supplements and biohacking interventions.
- Mental health: Mental illness is one of the most widespread and undertreated health burdens worldwide. In the U.S., nearly 1 in 5 adults(57.8 million people) experience a mental illness each year (NIMH). Globally, over 970 million people live with a mental disorder, with depression and anxiety accounting for the majority (IHME). Despite its prevalence, mental health services remain critically under-resourced: 70% of people with mental illness receive no treatment in low-income countries, compared to 35% in high-income countries (WHO Mental Health Atlas). As a result, mental illness not only reduces quality of life—it also increases mortality risk by 40–60%, especially when coexisting with chronic diseases (World Psychiatry).
Side note: Prevalence, Penetration, and Penetrance
When discussing health and disease, it’s important to distinguish between prevalence, penetration, and penetrance, as they describe very different concepts across public health and genetics. Prevalence refers to how common a condition is within a population—it’s a snapshot of disease burden. For example, if 15% of adults in a city have type 2 diabetes, the prevalence of diabetes is 15%. In contrast, penetration describes how far a health intervention (like a treatment, service, or technology) reaches its target population. If only 50% of people with diabetes in that city are receiving care, the treatment’s penetration is 50%. Penetration is often used in evaluating public health programs, showing whether people who need help are actually getting it.
Meanwhile, penetrance is a term from genetics and refers to something entirely different: the likelihood that someone who carries a disease-causing gene variant actually develops the disease. For instance, a BRCA1 mutation may have 65–80% penetrance, meaning not everyone with the gene will get cancer, but many will. While prevalence measures population-level disease, penetration measures how widely an intervention is delivered, and penetrance describes how reliably a gene leads to a trait or disease. Confusing these terms can lead to errors in health communication, policy design, or genetic risk interpretation—especially as precision medicine and public health increasingly intersect.
Who’s in The Most Danger?
When you identify the things that have the biggest effect on life and the things you’re lacking most, you can start to see what you should try and fix first.
- Young, Poor, and Severely Obese (The Triple Threat): Individuals who are under 40, in the bottom income quintile, and have BMI >35 face compounding risks: decades of potential life lost from obesity (up to 11.7 years for young Black males), systematic healthcare access barriers, and expanding income-based mortality gaps. Priority interventions: Weight management, financial stability through education/career development, and basic preventive care access.
- People in Conflict Zones and Dangerous Countries: Those living in areas with active warfare, extreme violence, or failed healthcare systems face immediate existential threats that dwarf all other health concerns. For example, if you have diabetes and are in the DRC and might be killed by a roaming war gang tomorrow, moving to safety from the war gang is the most important intervention—not optimizing your medication regimen. More than 70% of excess deaths in war zones occur from disrupted health systems, not violence itself (BMJ Global Health).Priority interventions: Relocation to safety, basic survival needs, emergency medical evacuation plans.
- Rural/Remote Populations with Limited Healthcare Access: Rural hospital closures (over 100 between 2013-2020) have forced residents to travel 20 miles farther for common services and 40 miles for specialized care. These populations face 25% fewer primary care physicians and 16% higher infant mortality rates in places like Appalachia. Priority interventions: Telemedicine setup, relocating closer to medical facilities, comprehensive preventive care during rare healthcare visits.
- People with Multiple Unmanaged Chronic Conditions: Individuals with 5+ chronic conditions lose 7.7 years of life expectancy, while those with 10+ conditions lose 17.6 years. Each additional unmanaged condition costs 1.8 years of life on average. Priority interventions: Intensive disease management (blood pressure control alone provides 27% mortality reduction), medication adherence, specialist care coordination. If you have poorly managed diabetes, hypertension, and heart disease, optimizing these provides years of life gained that completely dwarf trendy health intervention. Over 40% of U.S. adults have 2+ chronic conditions (CDC), so this applies to a large share of the population.
- Socially Isolated Individuals with Health Risks: Social isolation increases mortality risk by 33% (equivalent to smoking 15 cigarettes daily), particularly dangerous when combined with other health risks. Unmarried individuals face 28% higher mortality risk compared to married people. Priority interventions: Building social connections, community involvement, family relationship repair, professional mental health support.
- Untreated Mental Illness: Mental illness increases the risk of early death by 40–60%, often via suicide, substance use, or worsening chronic conditions (World Psychiatry). Globally, 70% of people with mental illness receive no treatment, especially in low-income countries (WHO Mental Health Atlas). This risk becomes even more deadly when combined with poverty, poor access to care, or social isolation.Priority interventions: Diagnosis and treatment access (e.g., teletherapy, community health), medication management, family engagement, and removing stigma.
- Elderly People in Poverty: The combination of advanced age, financial constraints, and typically multiple health conditions creates a perfect storm of vulnerability. This population often can’t afford medications, lives in unsafe housing, and lacks family support.Priority interventions: Social services navigation, medication assistance programs, fall prevention, social connection programs.
Step 4 - High Impact Interventions
We’ve made it. Here are the highest impact, most generally applicable health interventions for people living in developed nations (again, read above, but those living in certain parts of the world and at a higher health risk from certain dangers, like malaria or violence, would be better off focusing on other things, like buying nets or emigrating, than focusing on the recommendations below).
Sleep regularity emerges as one of the highest-impact interventions with medium effect sizes (Hedge’s g = -0.54), while resistance training shows one of the strongest mortality benefits (27% reduction at just 60 minutes weekly, PubMed, ScienceDirect). Recent meta-analyses reveal Mediterranean diet components deliver quantified health improvements, and social connections provide survival advantages comparable to smoking cessation (50% increased likelihood of survival, NCBI, Plos). Let’s start with sleep.
Sleep
Did we mention sleep enough yet? I think not. Sleep duration optimization represents perhaps the most undervalued health intervention in developed countries. Sleep duration follows a precise U-shaped mortality curve that rivals the most powerful cardiovascular medications. Meta-analyses of 1.5 million participants across 35 studies reveal optimal sleep duration of 7 hours, with each hour deviation increasing mortality risk. Chronic sleep restriction impairs glucose metabolism, increases hunger hormones, and significantly raises the risk of type 2 diabetes and obesity, independent of diet or exercise habits (Lancet Diabetes Endocrinology).
Three charts below, the first is an explanation of a Forest Plot from Nature (importantly note the middle line is the “line of no effect”), the second shows the relative risk of short sleep also from Sleep. Notice that across nearly every demographic, short sleep increases your chance of death.

Another fun chart below, from a review from the Journal of The American Heart Association that looked at 1673 studies to see the relationship between the length of sleep and certain health outcomes:
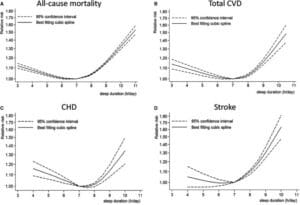
The numbers are staggering: sleeping 4 hours increases death risk by 7% (RR 1.07), while sleeping 11 hours increases risk by 55% (RR 1.55) (Nature).
These aren’t small effects. For comparison, most cardiovascular drugs celebrate 15-20% relative risk reductions, while sleep optimization provides effects that exceed nearly all pharmaceutical interventions.
- Sleep regularity emerges as potentially more important than duration alone. Studies show sleep regularity is a stronger predictor of mortality than sleep duration, yet this finding receives minimal public health attention. Irregular sleep patterns consistently associate with higher premature mortality risk across multiple population cohorts (OUP, Academic). Of course, there are confounders here, such as shift workers and people who have no control over when they go to bed and wake up, but controlled studies have shown dramatic benefits.
- Sleep Environment: Temperature control proves critical, with optimal sleep occurring between 17-28°C at 40-60% relative humidity (ScienceDirect). The WHO’s updated 2024 guidelines specify that noise should remain below 35 dB during sleep, with traffic noise cutoffs at 45 dB for roads, 44 dB for rail, and 40 dB for air traffic (ScienceDirect, NCBI). Each 10 dB increase correlates with 8-10% increased awakening probability. Complete darkness remains optimal, as even 5-10 lux exposure for two hours suppresses melatonin by 15-30% (PubMed).
- Caffeine and Alcohol: Caffeine cutoff times depend on dosing: standard coffee (107mg) requires consumption at least 8.8 hours before bedtime, while pre-workout supplements (217.5mg) need 13.2 hours (ScienceDirect). Alcohol disrupts REM sleep at all doses starting at 0.50 g/kg (approximately two drinks), with dose-response relationships affecting REM onset delay and duration reduction (ScienceDirect).
- Chronotype Optimization: Chronotype—the biological preference for sleeping and waking at certain times—affects everything from cognitive performance to metabolic health. Forcing a night owl into a 7 a.m. work schedule creates what’s known as social jet lag, a chronic misalignment between internal circadian rhythms and external demands that increases risk of obesity, depression, cardiovascular disease, and impaired glucose tolerance (Current Biology). Optimizing your schedule to match your chronotype—shifting work, workouts, or deep work blocks into biologically ideal hours—can improve energy, mood, and long-term health outcomes without changing total sleep time.
Exercise
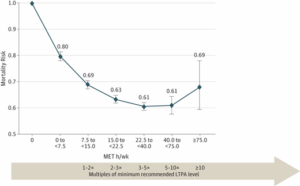
Mortality reduction data for physical activity rivals or exceeds most pharmaceutical interventions. Physically active individuals show 22-35% lower all-cause mortality versus sedentary individuals, with high-quality studies controlling for confounding factors demonstrating 0.4 to 4.2 years of life gained (NCBIPubMed). The dose-response relationship is remarkably consistent: 7 hours weekly of moderate activity provides 24% mortality reduction versus no activity (OUP Academic). Even 4-5 minutes daily of vigorous activity provides 26-30% mortality reduction—effects that would require multiple expensive medications to replicate (Nih). The chart below shows the relationship between leisure time physical activity (LTPA in MET hours, exercising during time that isn’t work time; 1 hour of running equals about 10 MET hours) and mortality, with the arrow on the bottom showing the multiple of minimum recommended (7.5 MET hours a week) and actual exercise. Controlled for education, disease, alcohol, and a few others from JAMA.
- Resistance training shows particularly impressive effects with relatively modest time investment. Meta-analytic evidence demonstrates 27% mortality reduction at just 60 minutes weekly (RR = 0.74, 95% CI: 0.64-0.86), with specific reductions in all-cause mortality (15%), cardiovascular mortality (19%), and cancer mortality (14%) (PubMed, ScienceDirect). The minimum effective dose requires only one set per muscle group weekly for detectable strength improvements, though 4-5 sets per week optimize strength gains (PubMed).
- Cardiovascular outcomes demonstrate NNT values of 37 for cardiovascular mortality prevention—exceptional effectiveness for a lifestyle intervention. 80% of aerobic exercise should be performed at low to moderate intensity (Zone 2), and 20% at high intensity (Zone 4–5). Zone 2 training, typically at 60–70% of maximum heart rate or just below the first lactate threshold, has been shown to enhance mitochondrial density, fat oxidation, insulin sensitivity, and endothelial function without the chronic stress of high-intensity work (Scandinavian Journal of Medicine & Science in Sports, Sports Medicine). A practical benchmark is the “talk test”—you should be able to comfortably speak 3–5 words per breath while exercising at this intensity. Sessions lasting 45–60 minutes, 3–4 times per week, have been shown to maximize aerobic adaptations, particularly mitochondrial biogenesis and capillary density, with relatively low injury risk (Journal of Biological Chemistry).
- High-intensity interval training (HIIT) delivers equivalent VO2max improvements (~18-19% increase over eight weeks) (PubMed) in approximately 50% the time compared to steady-state cardio (Nih). The optimal HIIT protocol involves four 4-minute intervals at 85-95% HRmax with 3-minute active recovery periods, limited to 2-3 sessions weekly to prevent overtraining.
-
Combined training provides additive mortality benefits. Resistance and aerobic training act on complementary physiological systems—muscle strength and cardiorespiratory capacity—and their combination yields a 40% reduction in all-cause mortality (RR = 0.60, 95% CI: 0.49–0.72), outperforming either alone (OUP Academic).
-
Exercise timing affects sleep and metabolic outcomes. Exercise timing affects both sleep and metabolic health. High-intensity workouts performed within four hours of bedtime delay sleep onset by 36–80 minutes (Nature Scientific Reports), while morning or early afternoon exercise poses no such disruption. In people with type 2 diabetes, afternoon exercise improves glycemic control significantly more than morning sessions (Savikj et al., Diabetologia, 2019).
- Sedentary Time: Prolonged sedentary behavior—particularly sitting for more than 8 hours per day—is independently associated with increased all-cause mortality, even among people who meet recommended exercise guidelines. Meta-analysis of over 1 million participants shows that those who sit the most have up to 59% higher risk of death, especially when physical activity is low (<5 minutes/day) (The Lancet). However, the risks are significantly reduced or eliminated when sedentary time is balanced with at least 60–75 minutes of moderate physical activity per day. It’s not just about moving more—it’s about sitting less. Incorporating regular movement breaks, standing desks, or short walks can offset the physiologic harm of long sitting bouts, especially for people with desk jobs.
The chart below shows the amazing power of exercise, post-diagnosis of diabetes, breast cancer, heart disease, and COPD. Those who exercise around ~40 METs per week (~5 hours of moderate exercise) have about half the mortality rate. Below is chart of Hazard Ratio (likelihood of bad event, in this case mortality) on the Y axis and PA MET-H/week (Physical activity, metabolic equivalent tasks, hours, per week; 1 hour of running is 10 METs compared to 1 hour of walking is 2.5 METs about) from the International Journal of Behavioral Nutrition and Physical Activity.
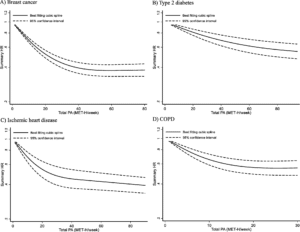
Food
The research reveal winners (as of now): Mediterranean dietary patterns reduce mortality by 20%, while ultra-processed foods increase death risk by 3% for every 10% of your diet they comprise. Most popular dietary fears—gluten, dairy, moderate red meat—show minimal health impact for most people, while the real gains come from emphasizing protective foods like extra virgin olive oil, fish, and minimally processed whole foods. Overall, however, food just scrapes into this category of high impact interventions. Only due to the sum of integrating all these interventions did it make it into this category. Exercise, sleep, and social life will provide greater benefit than any food intervention.
- Mediterranean diet research provides the strongest nutrition evidence base, anchored by the landmark PREDIMED randomized controlled trial. High adherence to Mediterranean diet patterns shows 4-47% (notice the big range, but this was a controlled trial) mortality reduction depending on baseline risk and adherence level (NCBI, ScienceDirect). Each 2-point increment in Mediterranean Diet Score provides 28% mortality reduction (HR: 0.72, 95% CI: 0.58-0.91). Theoretically, adoption at age 20 could add 13.0 years to male life expectancy and 10.7 years to female life expectancy. Even starting at age 60 provides 8.8 years additional life expectancy for males and 8.0 years for females (EatingWell).
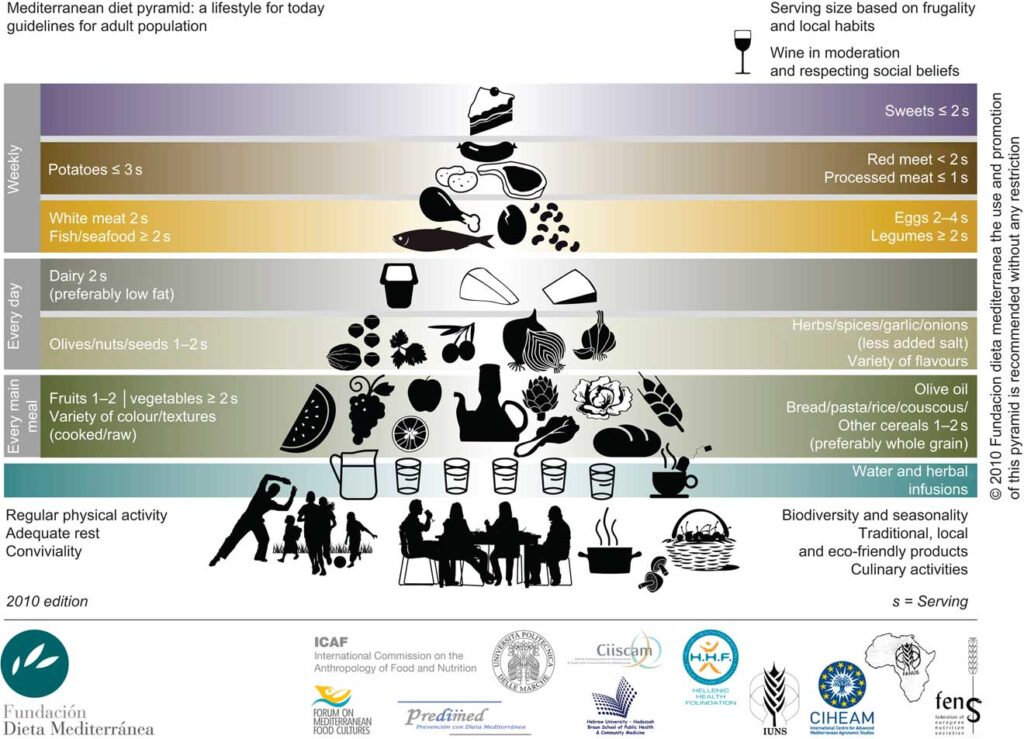
Side Note, certain oils seem to be “good”: High-quality EVOO consumption of 1.5 tablespoons daily associates with 34% lower all-cause mortality (HR 0.66, 95% CI: 0.49-0.89) through unique polyphenol compounds that provide anti-inflammatory effects similar to low-dose ibuprofen (Nature). The optimal dose is 20-25 mL daily, producing measurable blood pressure reductions of 1.44 mmHg diastolic and HDL cholesterol increases of 0.045 mmol/L (NIH).
Two servings of fatty fish weekly or 1,000-2,000 mg EPA+DHA daily reduces myocardial infarction risk by 13% (RR 0.87, 95% CI: 0.80-0.96), with a number needed to treat of 272 for preventing one heart attack over 3-5 years (NIH). C-reactive protein levels drop 26-41% with adequate omega-3 intake, while salmon, sardines, and anchovies provide high omega-3 content with minimal mercury exposure.
- Ultra-processed food reduction Every 10% increase in ultra-processed food consumption raises all-cause mortality risk by 3% (RR 1.03, 95% CI: 1.02-1.04) and cardiovascular mortality by 12% (American Journal of Preventive Medicine). Countries with high UPF consumption see 12-14% of premature deaths attributable to these foods, with sugar-sweetened beverages and processed meats showing the strongest mortality associations.
- Fiber and gut health: Each 10g daily fiber increase associates with 10% lower all-cause mortality (RR 0.90, 95% CI: 0.86-0.94), with optimal benefits around 25-35g daily from whole food sources. Americans consume only 15g daily—half the recommended amount—making fiber deficiency one of the most widespread nutritional inadequacies, easily corrected through emphasizing whole plant foods rather than isolated supplements.
- Food Fads (dairy, red meat, and gluten): Gluten avoidance provides no benefits for non-celiac populations; dairy consumption shows protective associations across 45 health outcomes; moderate red meat (1-2 servings weekly) carries minimal risk with only 1-6 fewer events per 1000 people when reduced; and vitamin supplements provide no mortality benefits for well-nourished adults despite $30 billion annual spending (Nature). The real gains come from increasing protective foods rather than eliminating traditionally consumed items.
Social Life
One in three adults over age 45 reports feeling lonely, and social isolation is as strong a predictor of early death as obesity, smoking, or inactivity—yet it receives a fraction of the attention (CDC, 2020).Social connections rank among the most powerful predictors of health and longevity, with mortality benefits rivaling smoking cessation (Nih). Strong social relationships provide a 50% increased likelihood of survival (OR = 1.50, 95% CI: 1.42-1.59), (Plos), while social isolation increases all-cause mortality risk by 32-35% (PubMed) (HR = 1.33, 95% CI: 1.26-1.41) (Plos).
The evidence overwhelmingly demonstrates that social connections are not just “nice to have” but represent a fundamental determinant of health and longevity. Recent meta-analyses spanning 1.3 million individuals across 36 studies show social isolation carries a hazard ratio comparable to smoking, with effects consistent across different measurement tools, income levels, and geographic regions (Plos). While most studies are observational and subject to confounding (for example, sicker people may withdraw socially), the consistency and dose-response pattern strengthen the causal argument—and randomized interventions show meaningful improvements in well-being and mortality. The relationship follows a clear threshold pattern: even monthly meaningful social contact appears sufficient for health benefits, while complete isolation combined with living alone increases mortality risk by 77%.
Chronic loneliness increases cortisol, reduces immune function, elevates inflammatory cytokines, and worsens cardiovascular risk markers, essentially accelerating biological aging (Hawkley & Cacioppo, Nature Reviews Neuroscience).
- The Danger of Living Alone: Think of social connection like a light switch, not a dimmer. UK Biobank data from 458,146 participants shows that people who never have social visits face a 39% increased mortality risk (HR = 1.39, 95% CI: 1.30-1.49), while just quarterly contact drops this to 11% increased risk (Biomedcentral). The real danger zone? Living alone with no social visits creates a 77% increased mortality risk (HR = 1.77, 95% CI: 1.61-1.95)—that’s like adding 15 years to your biological age (PubMed). Even daily visits can’t fully offset living alone, so the combination of structural isolation (no people around) plus functional isolation (feeling lonely) creates multiplicative, not additive, health risks.
- Marriage works like a longevity drug, but men get double the dose. Married people reduce their all-cause mortality risk by 12-24%, with married individuals showing odds ratios of 0.88 (95% CI: 0.85-0.91) compared to unmarried folks (Wiley Online Library). But here’s the kicker: divorced or separated men face a 37% increased mortality risk (HR = 1.37, 95% CI: 1.27-1.49) while divorced women only face 22% increased risk (HR = 1.22, 95% CI: 1.13-1.32) (Nih). Why? Men typically rely on their spouse as their primary social support system, while women maintain broader friendship networks that provide backup protection. Think of marriage as men’s social insurance policy—when it’s gone, they’re often left without a safety net.
- Volunteering has an optimal dose: 1-10 hours monthly prevents one death per 18-20 volunteers. Meta-analyses show volunteers have a 22% lower mortality risk (RR = 0.78, 95% CI: 0.66-0.90), creating a Number Needed to Treat of 18-20 people volunteering to prevent one death over 5-7 years (PubMed). But like exercise, more isn’t always better—mental health benefits peak at 1-10 hours monthly, with burnout effects kicking in above 10 hours (Springer). The sweet spot appears to be weekly commitment rather than sporadic marathon sessions, suggesting your brain needs consistent social engagement more than intense bursts of do-gooding.
- Face-to-face beats Facebook, but dogs beat being alone—especially if you’re single. Digital connections provide some benefits through active engagement (posting, commenting) but passive social media use increases anxiety in 80% of studies with effect sizes around r = 0.08 (Liebert). Meanwhile, dog ownership reduces all-cause mortality by 24% and cardiovascular death by 31%, with single-person households seeing the biggest benefits: 33% lower all-cause mortality (HR = 0.67, 95% CI: 0.65-0.69) (AHAJournals). Dogs force you into regular exercise through walks, provide emotional support comparable to human relationships, and create social opportunities with other dog owners—essentially acting as a social connection multiplier.
- Workplace friendships deliver measurable ROI: burnt-out employees show 68% lower productivity. Workplace social connections create effect sizes of d = 0.2-0.5 for wellbeing, while loneliness costs UK employers £2.5 billion annually through reduced productivity (NIH). Social support programs in healthcare settings show 20% increased odds of survival compared to standard medical treatment alone, while mindfulness interventions demonstrate effect sizes of Cohen’s d = -0.60 for stress reduction (ResearchGate). The business case is clear: investing in workplace social connection isn’t just nice-to-have team building—it’s a productivity and retention strategy with quantifiable returns.
- Age, gender, personality, and cultural factors create substantial variation in how social connections affect health. Older adults (60+) show 50% risk of social isolation with one-third experiencing loneliness, WHO while effect sizes vary by age with longer follow-up periods showing stronger mortality associations in older populations. BiomedcentralSpringerLink Social activities demonstrate gender-specific protective effects against dementia risk, with women showing greater absolute mortality reductions from social interventions.
- Effective social interventions exist but require personalized, multi-component approaches lasting 1-4 years. Systematic reviews show social isolation interventions achieve effect sizes of SMD = 0.63 (95% CI: -0.10 to 1.36) for loneliness reduction, with 72-84% chance of improvement versus usual care (NCBI). The most successful programs combine multiple elements: group-based meetings (8-10 weekly sessions), art or physical activity components, and integration with existing healthcare systems. Cost-effectiveness analyses show most programs cost less than $50,000/QALY, with community-based interventions ranging from cost-saving to $38,300/QALY over 20 years—making social connection programs among the most cost-effective health interventions available.
What to Quit: alcohol, smoking, inactivity, and being alone
- Alcohol: For decades, red wine was marketed as heart-healthy. But recent data overturns this idea completely. Even low levels of alcohol consumption (1–2 drinks per day) are now linked with increased risks of hypertension, atrial fibrillation, breast cancer, and early death. A massive 2018 analysis in The Lancet found no safe level of alcohol, showing a linear relationship between alcohol intake and all-cause mortality (Lancet, 2018). The World Health Organization officially updated its guidance in 2023 to state that any amount of alcohol carries health risk—not just heavy drinking. Moderate drinkers face a 14% increased risk of cancer, and daily drinkers may shave years off their life expectancy. If alcohol were discovered today, it would likely be regulated as a carcinogen.
- Smoking: Tobacco kills more people than any other modifiable risk factor, accounting for 480,000 deaths annually in the U.S. alone (CDC). Quitting before age 40 reduces 90% of the excess mortality risk compared to continuing smokers (NEJM, 2013). Even for those who quit later in life, life expectancy improves almost immediately. Vaping may be less harmful than cigarettes, but it still carries cardiovascular and pulmonary risks, especially in youth. There is no safe form of tobacco. Unlike many health interventions that work slowly, smoking cessation creates almost immediate reductions in heart attack and stroke risk, making it one of the highest-yield choices a person can make.
- Inactivity: Prolonged sitting—especially more than 8 hours a day—raises your risk of early death by 10–20%, even if you exercise regularly. Meta-analyses in the Annals of Internal Medicine found that sitting for long periods without breaks leads to higher rates of heart disease, diabetes, and cancer (Annals of Internal Medicine, 2015). The problem isn’t just lack of exercise—it’s excessive sedentary time. Even those who work out can’t “undo” the biological harms of a sedentary workday. The fix? Break up sitting every 30–60 minutes with a short walk, 60 seconds of bodyweight movement, or standing posture. The best health benefits don’t just come from the gym—they come from building movement into every hour of your day.
- Social Isolation: Loneliness and social isolation increase your risk of heart disease by 29% and stroke by 32%, levels comparable to smoking and obesity (Heart, 2016). In a meta-analysis of over 3.7 million people, social isolation was linked to a 26–32% increase in all-cause mortality (PLOS Medicine, 2015). The mechanism appears to involve both behavioral (less exercise, more alcohol) and biological (elevated cortisol, inflammation) pathways. Despite being harder to measure, loneliness affects cardiovascular health just as powerfully as smoking a pack a day. Regular in-person interactions, strong friendships, group exercise, volunteering, or even weekly phone calls can all dramatically reduce risk. Your relationships aren’t just nice—they’re medically necessary.
Preventive Care & Chronic Disease Management
Healthcare systems spend 97% of budgets treating diseases reactively instead of preventing them or managing them optimally—yet the highest-impact interventions are often the simplest and cheapest.
Blood pressure control, diabetes management, and cholesterol optimization prevent more deaths than most expensive procedures, while cancer screening and vaccination provide quantifiable mortality benefits with excellent cost-effectiveness ratios. The interventions that work best have something in common: they target the leading causes of death (cardiovascular disease, cancer, infections) with interventions that have been tested in massive randomized trials with clear, measurable outcomes.
The problem isn’t that we don’t know what works—it’s that healthcare systems remain incentively biased toward expensive treatments over simple prevention and management.
- Blood pressure control delivers the strongest mortality benefits of any medical intervention—every 10 mmHg reduction prevents major cardiovascular events within 2-3 years. Lowering systolic blood pressure by 10 mmHg reduces cardiovascular events by ~20%, stroke by ~27%, and all-cause mortality by ~13% within 2–3 years. The landmark SPRINT trial showed targeting <120 mmHg vs. <140 mmHg lowered all-cause mortality by 27% (HR 0.73; 95% CI 0.60–0.90) with a Number Needed to Treat of ~83 over 3.7 years (NEJM). Current guidelines recommend <130/80 mmHg for high-risk patients and <140/90 mmHg for adults ≥65 (ACC). The remarkable part? Lifestyle modifications alone (weight loss, sodium reduction, exercise) can achieve 5-15 mmHg reductions, often eliminating the need for medication entirely while providing benefits comparable to most pharmaceutical interventions.
- Diabetes management with HbA1c targets <7.0% prevents complications and saves lives—but early intervention is everything. Maintaining HbA1c <7% reduces microvascular complications by 37%, myocardial infarction by 14%, and all-cause mortality by 21% according to ADA-endorsed clinical trials (Diabetes Care). The ADA 2024 guidelines emphasize personalized targets based on age, comorbidities, and life expectancy, with monitoring at least twice yearly if meeting goals (Cardiometabolic Health). The key insight? Early intervention provides microvascular benefits within 1–2 years but requires 10+ years to show cardiovascular benefits—meaning aggressive early management pays dividends decades later. Annual monitoring minimum for prediabetes (5.7-6.4% range) catches progression early when lifestyle interventions are most effective.
- Cholesterol management follows a simple rule: every 38.7 mg/dL LDL-C reduction provides 21% cardiovascular risk reduction, regardless of baseline levels. The 2018 AHA/ACC guidelines recommend <100 mg/dL for primary prevention and <70 mg/dL for secondary prevention, with very high-risk patients targeting <55 mg/dL (AAFP). Every 38.7 mg/dL (1 mmol/L) LDL-C reduction provides 21% ASCVD risk reduction, with statin therapy achieving 30-50% LDL-C reductions (Circulation). Unlike blood pressure where “normal” varies by person, LDL cholesterol follows a “lower is better” relationship with no threshold—meaning aggressive treatment in high-risk individuals provides proportional benefits. Cost-effectiveness ranges from $3,000-$50,000 per QALY depending on baseline risk, making this intervention a healthcare bargain for most adults over 40.
- Cancer screening hits different effectiveness sweet spots—colonoscopy dominates, mammography starts earlier, lung screening targets the right smokers. Colonoscopy prevents ≈24–28 cancer deaths per 1,000 individuals screened over a lifetime with a Number Needed to Screen (NNS) of ≈300–400 over 15 years (NCBI). Current USPSTF guidelines recommend screening from age 45-75 with 10-year intervals. Cost-effectiveness varies by method: annual FIT testing costs $3,811-$5,384 per person, while 10-year colonoscopy costs $5,375-$7,031 per person (Science Direct). Mammography screening benefits from 2024 USPSTF updates lowering starting age to 40, with the hybrid strategy (annual 45-55, then biennial to 75) costing ~$40,000/QALY (PubMed). Lung cancer screening for ages 50+ with ≥20 pack-year smoking history shows NNS ≈130 with cost-effectiveness of $39,000–$76,000/QALY (USPSTF, Nature).
- Vaccination schedules deliver measurable protection with clear dosing strategies that have prevented millions of deaths. COVID-19 vaccines follow age-specific recommendations: all adults ≥18 get updated vaccines, while adults ≥65 and immunocompromised individuals get two doses separated by 6 months, showing 33% effectiveness for emergency department visits and 45–46% effectiveness for hospitalizations (CDC). Annual flu shots achieve 36–54% effectiveness in outpatient settings, with high-dose and adjuvanted vaccines preferred for adults ≥65 showing superior protection (CDC). Major updates: pneumococcal vaccination age dropped from 65 to 50 in October 2024, with PPSV23 showing 60–70% effectiveness against invasive disease (CDC). Shingrix provides 10+ years of protection plus emerging evidence of ~17% reduced dementia risk compared to old Zostava ( NCOA).
- Risk factor clustering multiplies benefits exponentially—managing blood pressure, cholesterol, and diabetes together prevents more events than treating each separately. High-sensitivity CRP levels >3 mg/L indicate increased cardiovascular disease risk beyond traditional factors, helping guide primary prevention strategies for intermediate-risk individuals. The concept of “cardiovascular risk equivalents” means that diabetes, chronic kidney disease, or multiple risk factors create the same risk as having already had a heart attack—justifying aggressive intervention. Polypill strategies combining low-dose aspirin, statin, and ACE inhibitor show 20–30% cardiovascular event reduction in high-risk populations, with cost-effectiveness ratios of $10,000–$30,000 per QALY (The Lancet). The multiplicative effect explains why comprehensive risk factor management provides such dramatic benefits compared to single-intervention approaches.
- Dental health creates quantified systemic disease connections, but causation remains murky despite strong correlations. People with gum disease face ~20% higher risk of heart attack and stroke, with meta-analyses showing increased cardiovascular risk (RR = 1.20, 95% CI 1.14-1.26) in patients with periodontitis (American Journal of Medicine). A 2024 study of hemodialysis patients showed preventive dental care reduced cardiovascular risk by 14%, acute myocardial infarction by 21%, and pneumonia by 26% (Nature). Men show higher risk than women, with odds ratios of 1.22 vs 1.11 for cardiovascular disease (NIH). However, while strong correlations exist, limited evidence demonstrates that treating dental disease directly prevents cardiovascular events—it’s association, not proven causation (Harvard Health). Still, good oral hygiene is cheap insurance with potential systemic benefits.
- General health checkups detect substantial disease but show mixed evidence for mortality benefits—the screening paradox strikes again. Annual screening per 10,000 people detects 1,185 cases of prediabetes, 287 cases of diabetes, 73 cases of chronic kidney disease, and 669 positive colorectal screens—with 28% of diabetes cases and 89% of kidney disease cases previously unrecognized (AJMC). But meta-analysis of 17 randomized trials with 251,891 participants found no significant reduction in all-cause mortality or cardiovascular events from general health checks (NCBI). This paradox—increased disease detection without mortality benefit—suggests that unfocused health checks may be less valuable than targeted screening for specific conditions in appropriate populations. The lesson? Detection doesn’t automatically equal prevention—you need evidence-based interventions that actually change outcomes.
- Genetic testing enables personalized medicine but requires careful cost-benefit analysis—family testing beats population screening by massive margins. Cascade testing in families with hereditary cancer or heart disease costs ~$6,100–$9,500/QALY—far more cost-effective than population-wide genetic screening at ≈$68,600/QALY (VUMC News). BRCA testing in affected women costs AU$18,900 per QALY, while cascade testing of family members costs only AU$9,500 per QALY incrementally (Science Direct). Preimplantation genetic testing shows favorable ratios of $14,242 per QALY (BRCA1) and $12,893 per QALY (BRCA2) (NIH). The variability ranges from $344 to $2.5 million per QALY depending on population characteristics, emphasizing that appropriate patient selection makes or breaks genetic testing value (PubMed). When used correctly, genetic testing supports personalized medicine without wasting resources.
Side Note, Screening Paradox:
The screening paradox highlights a central tension in preventive medicine: while early detection can save lives, screening often finds more disease than it prevents deaths from. Across major screening programs, 20–50% more disease cases are diagnosed than lives saved—leading to a surge in unnecessary treatments, false positives, and real patient harm.
-
Mammography: For every 2,000 women screened over 10 years, just 1 breast cancer death is prevented, while 10 women are overdiagnosed and treated unnecessarily (UK Independent Panel). That’s a 19% overdiagnosis rate with 0.05% absolute mortality reduction despite 20% relative risk reduction. Up to 60% of women undergoing 10 years of annual mammography experience at least one false positive, often leading to biopsies or follow-up imaging. These events cause lasting anxiety and reduced trust in care in ~30% of patients (Elmore et al., JAMA).
-
PSA screening for prostate cancer: Prevents 1.3 deaths per 1,000 men screened over 13 years, but results in 23–42% overdiagnosis rates, and requires 781 men to be screened to prevent one death (USPSTF). After PSA screening, as many as 1 in 3 men develop urinary incontinence, and 2 in 3 experience long-term erectile dysfunction—often for slow-growing tumors that would never have caused symptoms (Wilt et al., NEJM).
-
Lung cancer screening (low-dose CT): Saves 3–4 lives per 1,000 people screened, but with 18.5% overdiagnosis, 250–320 needed to screen per death prevented, and 24.2% false positive rate—three times higher than chest X-rays (NLST Trial, N Engl J Med). In the NLST trial, 7% of people with false-positive lung scans underwent invasive diagnostic procedures (e.g., bronchoscopy or biopsy) for benign nodules (NLST). Repeated CT scans can raise long-term cancer risk. Estimates suggest 1–2% of U.S. cancers may stem from medical imaging exposure (Brenner & Hall, NEJM).
-
Thyroid cancer in South Korea: Between 1993–2011, diagnoses increased 15-fold with no mortality reduction. 97% of these cases were clinically insignificant, slow-growing tumors that never needed treatment (Ahn et al., NEJM). Unnecessary thyroidectomies resulted in permanent hypocalcemia (6–12%) and vocal cord damage (0.9–2%), plus lifelong medication needs
Here’s the remarkable truth: five evidence-based interventions can add 10-15 years to your life expectancy while costing less than most people spend on coffee. Sleep optimization (7 hours nightly with consistent timing) reduces mortality risk by 12-55% depending on your current habits. Exercise—just 60 minutes weekly of resistance training plus 150 minutes of moderate cardio—delivers a 27% mortality reduction that exceeds most pharmaceutical interventions. Mediterranean diet patterns provide 4-47% mortality reduction, while strong social connections offer a 50% increased likelihood of survival (comparable to quitting smoking). Finally, basic preventive care like blood pressure control (every 10 mmHg reduction prevents major cardiovascular events within 2-3 years) and cancer screening delivers quantifiable mortality benefits with excellent cost-effectiveness ratios under $50,000 per quality-adjusted life year.
What would I do first if everything was out of whack? Start with sleep regularity—same bedtime and wake time for two weeks, aiming for 7 hours nightly. Add a 20-minute walk three times weekly, progressing to basic bodyweight exercises (pushups, squats, planks) for 10 minutes twice weekly. Swap one processed meal daily for whole foods: olive oil, fish (if I wasn’t allergic…), vegetables, legumes. Schedule one meaningful social interaction weekly—coffee with a friend, volunteering, or calling family. Stop smoking, excessive alcohol drinking, sitting, and being alone. Finally, keep your chronic medical health conditions under the best control you can.
These aren’t complicated interventions requiring expensive supplements or exotic protocols—they’re the fundamentals that actually move the needle on health outcomes. The pharmaceutical industry spends billions marketing complex solutions, but the highest-impact interventions remain embarrassingly simple, essentially free, and available to everyone starting today.
Step 5 - Mid-tier Interventions
Your doctor recommends generic metformin for $4 per month with rock-solid evidence for diabetes prevention. Meanwhile, your biohacker friend swears by $150 monthly NMN supplements based on mouse studies. This perfectly captures the mid-tier intervention dilemma: promising mechanisms, plausible benefits, but questionable cost-effectiveness and efficacy compared to proven basics.
The Bridge Between Foundation and Folly
Important Context: These are mid-tier interventions—the extras you consider AFTER mastering the high-impact fundamentals from Step 4. Basic safety, sleep optimization, exercise, diet, social connections, and preventive care provide 80% of health benefits at 20% of the cost. These interventions deliver the remaining 20% of benefits, often at 5-20x the price.
Think of mid-tier interventions like luxury car features. Heated steering wheels provide real comfort, but they’re hardly essential when your engine needs basic maintenance. The wellness industry profits by selling heated steering wheels to people whose cars won’t start.
Evidence-Based Supplements (The Foundation)
Before diving into experimental territory, these supplements have the strongest evidence bases—though still modest compared to lifestyle interventions.
- Vitamin D: The Deficiency Corrector
Only worth supplementing if you’re actually deficient (most people in northern climates are). Systematic reviews show benefits for bone health, immune function, and mood, but minimal benefits in those with normal levels. Cost: $5-15/month. Test first—supplementing without deficiency wastes money. - Creatine: The Performance Enhancer
Over 717 studies show 5-15% improvement in high-intensity exercise performance, increased strength and muscle mass, potential cognitive benefits in elderly. Daily cost: $0.20-0.30. One of the few supplements with genuinely robust evidence across multiple populations. - Omega-3s: The Targeted Approach
16.5% reduction in hospitalization rates for high-risk cardiovascular populations, but minimal benefits in healthy individuals with adequate fish intake. Cost: $0.50-1.50 daily. Better to eat fish twice weekly unless you have documented deficiency or high cardiovascular risk. - Protein Powder: The Convenience Food
Not technically necessary if you hit 0.7-1g protein per pound bodyweight through whole foods, but convenient for busy lifestyles. Meta-analyses show muscle protein synthesis benefits, but whole food protein sources provide additional nutrients. Cost: $30-50/month. Choose based on convenience, not necessity. - Magnesium: The Sleep Aid
Moderate evidence for sleep quality improvement and blood pressure reduction. About 50% of people consume inadequate dietary magnesium. Cost: $10-25/month. Most beneficial for those with poor sleep or documented deficiency. - Vitamin C: The Immune System Myth
Large meta-analyses show no significant reduction in common cold incidence for general population, modest duration reduction (~8% in adults). Better obtained from citrus fruits and vegetables. Supplementation largely unnecessary except for extreme athletes or those with severe dietary restrictions. - Collagen: The Beauty Industry Darling
Small studies suggest modest skin elasticity improvements, but effect sizes are minimal and study quality varies. Cost: $25-50/month. Your body makes collagen from any protein source—eating adequate protein with vitamin C likely equivalent at fraction of cost.
Free Interventions (Cost: Time Only)
- Nature Exposure: The 120-Minute Rule The research reveals a striking threshold effect: spending 120+ minutes per week in nature provides significant health benefits (UK study, n=19,806). Meta-analysis shows stress reduction effects (d = -0.35, 95% CI [-0.55, -0.14], p = 0.0009) with $0 investment versus ~$30,000 equivalent value in mental health benefits annually. These effects peak at 300 minutes. Japan loves this so much they have stressed people take “nature baths,” and they work.
- Sunlight: Beyond Vitamin D
Mid-day sun exposure (25-30 minutes, 25% body surface area) produces vitamin D changes that can’t be replicated with pills—increasing 25(OH)D from 59 to 84 nmol/L in 6 weeks, plus triggering nitric oxide release for blood pressure reduction. Meta-analyses show cardiovascular mortality benefits, but skin cancer risk creates a U-shaped curve requiring individual calibration. - Cold Exposure: The 11-Minute Protocol
Despite popular enthusiasm, meta-analysis of 11 studies shows the total weekly requirement is just 11 minutes—not per session, but total. Protocol: 2-4 sessions of 1-5 minutes each, water temperature 45-60°F. 29% reduction in sickness absence observed, but deliberate cold exposure differs dramatically from ambient cold, which increases cardiovascular mortality. - Breathing Techniques: The Parasympathetic Hack
Meta-analysis of 31 RCTs shows effect sizes for depression (g = -0.40) and anxiety (g = -0.32) that compete with SSRIs, at zero monetary cost. Optimal parameters: <10 breaths per minute, 5-20 minutes daily for clinical benefits through respiratory-cardiac coupling enhancement. Meditation can help you get here.
Equipment-Dependent Interventions
- Red Light Therapy: The Mechanistic Darling
The biological mechanism sounds compelling: specific wavelengths (660-850nm) enhance mitochondrial ATP production. 7 clinical trials show modest skin improvements, but Cleveland Clinic states “not enough evidence to support most uses”. Equipment cost: $200-2,000+ for benefits that a $50 monthly gym membership would likely exceed. The evidence is poor here. Critical assessment: The gap between elegant cellular mechanisms and meaningful clinical outcomes remains vast. Most studies are small, short-term, and industry-funded. - Infrared Saunas: The Cardiovascular Substitute
Extremely limited evidence from only 9 papers, mostly from the same research groups, shows potential cardiovascular benefits for specific populations—particularly congestive heart failure patients. Cost: $1,000-10,000+ for home units versus $20-40/session at gyms. For healthy individuals, a 20-minute walk provides superior cardiovascular benefits with zero equipment cost and stronger evidence.
Mid-Tier Supplement Analysis
Beyond the evidence-based basics, the supplement landscape becomes a minefield of modest benefits at exponential costs. Most effect sizes here are small-to-moderate at best, often seen only in specific populations or conditions.
- Berberine: The “Natural Metformin”
This represents the strongest evidence in the experimental supplement category, but still falls short of pharmaceutical standards. Total cholesterol reduction SMD = -1.06 (95% CI: -1.48, -0.64, p<0.001), glucose control improvements, and liver health benefits. Cost: $20-40/month versus $4-8/month for generic metformin with superior evidence and safety data. Critical reality check: Works best in metabolically dysfunctional populations, shows minimal benefits in healthy individuals. Why choose the more expensive option with less safety data when proven pharmaceuticals exist? - CoQ10: The Fatigue Fighter
Meta-analysis of 13 RCTs shows genuine but modest fatigue reduction (Hedges’ g = -0.398, NNT ~7-10). Optimal dose: 200-300mg daily. Cost: $20-40/month. The mechanism is sound, but it works best for unexplained fatigue after ruling out correctable causes like poor sleep, stress, or nutritional deficiencies—which should be addressed first. - Curcumin: The Absorption Problem
Anti-inflammatory effects on biomarkers are real, but the ~1% bioavailability without enhancement makes most products ineffective. Triglyceride reduction -19.1 mg/dL sounds impressive until you realize an anti-inflammatory diet achieves better results at zero additional cost. - The NAD+ Precursor Hype (NMN/NR)
This represents pure marketing triumph over science. Meta-analysis of 12 studies shows NAD+ elevation but zero meaningful clinical endpoints—no improvements in glucose, lipids, or functional measures. Cost: $50-150/month for what amounts to expensive urine. The mouse studies remain compelling, but human translation has completely failed.
Borderline Interventions
- Chiropractic Care: The Back Pain Specialist
Evidence supports use for specific conditions but often oversold. Professional organizations now recommend spinal manipulation for acute low back pain: pain reduction 1.38 points on 10-point scale, healthcare cost savings. Small stroke risk with neck manipulation, though evidence quality is low. Critical context: Works for acute/subacute musculoskeletal pain. Claims about “subluxations,” systemic health, or chronic conditions lack evidence. Stick to evidence-based practitioners for specific pain conditions only. - Acupuncture: The Pain Management Tool
Systematic reviews show genuine but modest chronic pain benefits: effect size SMD -0.61 (95% CI -0.76 to -0.47). Best evidence for chronic pain, osteoarthritis, migraine. Cost: $75-150 per session. Reality check: 40-70% show meaningful improvement—meaning 30-60% see no benefit. Effects typically last 1-6 months. Best used as adjunct to conventional care for specific conditions, not general wellness. - Meditation: The Mental Health Powerhouse
This stands out as genuinely evidence-based with effect sizes rivaling pharmaceutical treatments. Comprehensive analysis of 44 meta-analyses (30,483 participants) shows robust effect sizes (d = 0.10-0.89) vs. passive controls. Comparable to CBT for chronic pain, similar efficacy to psychotherapy for depression/anxiety. Cost: $0-15/month for apps. Unlike most interventions in this tier, meditation becomes more cost-effective over time as skills develop, shows neuroplasticity changes, and provides cumulative benefits. This deserves consideration even for those with optimized fundamentals.
Experimental Interventions
“Experimental” was the kindest word I could think of…
- Grounding/Earthing: The Electron Theory
Approximately 20 small studies with mostly subjective measures. Sample sizes typically 10-58 participants, lack proper controls. Proposed mechanism lacks robust scientific foundation. High susceptibility to placebo effects. - Hydrogen Water: The Antioxidant Approach
Meta-analysis shows lipid improvements (total cholesterol, LDL, triglycerides, p=0.01). Limited evidence from small-scale studies. Cost: $30-100/month with stability and dosing limitations.
Side Note: The Placebo Problem
Imagine you’re testing a new pill to treat chronic knee pain. You recruit 200 people who all have similar levels of pain. Half of them get the real drug, and the other half get a placebo—a pill that looks exactly the same but has no active ingredients (just sugar and filler). The participants don’t know which pill they’re getting. Neither do the doctors checking their pain scores—this is called a double-blind randomized controlled trial.
After 6 weeks, you find that both groups report feeling better. In fact, the placebo group reports a 40% reduction in pain, even though they didn’t get the real medication. This is the placebo effect—patients’ beliefs, expectations, and the clinical environment trigger real brain responses (like releasing natural opioids and dopamine) that change their experience of pain.
These trials show why we can’t trust stories or before-and-after testimonials. Without a placebo control group, you might think the drug works—when really, people just got better because they believed they would. That’s why every credible treatment in medicine must outperform a placebo in controlled trials. If it doesn’t, it’s not medicine—it’s marketing.Meta-analysis of 186 trials reveals 54% of treatment effects attributable to contextual/placebo factors. Placebo effects vary: 30-60% for pain, large effects for depression, and minimal for objective measures. The wellness industry systematically exploits this through elaborate rituals, expensive pricing, and impressive-sounding mechanisms.
Remember our evidence pyramid? The best studies are “controlled” (by placebos) to see if our interventions are comparably effective.
Overhyped Interventions
- Detox Programs: The $8 Billion Mythology
2015 systematic review found “no compelling research to support detox diets”. Human bodies already possess sophisticated detoxification systems that function effectively without intervention. Weight loss occurs through calorie restriction, not detoxification. Cost: $30-500+ with safety concerns including electrolyte imbalances. - IV Vitamin Therapy: The $3 Billion Hydration Theater
Mayo Clinic analysis found “limited evidence” for benefits in healthy people. 2020 Canadian systematic review found “no evidence-based guidelines”. Cost: $100-400 per session. Oral supplements show equivalent absorption when properly dosed. - Peptides: The $35 Billion Gray Market
Most peptides are not FDA-approved for human use. BPC-157 has animal studies only, no human RCTs. Cost: $2,000-10,000+ annually with unstudied long-term effects and contamination risks.
The Economics of Marginal Gains
The fundamental mathematics of mid-tier interventions reveals an uncomfortable truth: They typically cost 5-50x more than foundational interventions while delivering 10-50% of the benefit. This isn’t necessarily a problem for wealthy individuals who’ve optimized basics, but it represents poor resource allocation for most people.
Consider a concrete example: A person spending $200 monthly on NMN, red light therapy, and IV vitamins could instead invest in:
- High-quality gym membership: $50/month
- Organic food upgrade: $100/month
- Sleep optimization (mattress, blackout curtains): $50/month amortized
- Stress management coaching: $0-50/month
The evidence strongly favors the latter approach, yet the wellness industry’s marketing machine consistently promotes the former.
Individual Variation: The Personalization Challenge
Mid-tier interventions show extreme individual variation that’s often predictable based on baseline characteristics:
- Metabolic supplements (berberine, curcumin) work best in metabolically dysfunctional populations, showing minimal benefits in healthy individuals.
- Stress-management interventions (ashwagandha, meditation) provide greatest benefits for those with elevated baseline stress, anxiety, or cortisol levels.
- Recovery modalities (massage, cold exposure, saunas) show enhanced benefits in athletes and highly active individuals versus sedentary populations.
- Pain management approaches (acupuncture, chiropractic) work best for specific conditions with clear diagnostic criteria rather than general wellness applications.
The personalization principle: Mid-tier interventions function more like targeted therapeutics than general wellness tools. They’re most effective when matched to specific deficits or conditions rather than used broadly.
The Mid-Tier Decision Tree
Tier 1: Consider Only After Optimizing Basics
- Nature exposure (if sedentary lifestyle)
- Sunlight optimization (if vitamin D deficient)
- Breathing techniques (if chronically stressed)
- Meditation (if mental health challenges)
- Quality supplements (vitamin D, omega-3, magnesium, creatine)
Tier 2: Targeted Applications Only (iffy)
- Berberine (if metabolically dysfunctional and metformin contraindicated)
- CoQ10 (if unexplained fatigue after medical evaluation)
- Chiropractic (if acute/subacute back/neck pain)
- Acupuncture (if chronic pain conditions)
Tier 3: Proceed with Extreme Caution
- Most expensive supplements (NMN, peptides)
- Biohacking devices without clear indication
- IV therapy for wellness (not medical conditions)
- Detox programs (avoid entirely)
The 80/20 Health Investment Principle
80% of health benefits come from 20% of possible interventions: sleep optimization, exercise, nutrition fundamentals, stress management, and social connections. Mid-tier interventions can provide the remaining 20% of benefits, but typically at 5-20x the cost.
For most people, time and money are better invested in perfecting the fundamentals rather than pursuing marginal optimization through expensive mid-tier interventions.
Before considering any mid-tier intervention, honestly evaluate:
- Have you talked to your doctor? (They know you much better than a random guy on the internet)
- Have you optimized sleep? (7-9 hours, consistent schedule, sleep hygiene)
- Is your diet fundamentally sound? (adequate protein, vegetables, minimal ultra-processed foods)
- Are you exercising regularly? (150+ minutes moderate activity weekly)
- Is stress management in place? (social support, relaxation practices, work-life balance)
- Are basic supplements addressed? (vitamin D if deficient, others based on testing)
Only after honest “yes” answers to these questions do mid-tier interventions become reasonable considerations.
The mid-tier represents the frontier where health optimization meets diminishing returns. These interventions can provide genuine benefits, but they require careful selection based on individual needs, strong evidence evaluation, and realistic cost-benefit analysis. The wellness industry profits by reversing this priority order—selling expensive optimizations to people whose fundamentals need attention.
Step 6 - Use it in Real Life
Imagine two people after reading this guide: Sarah meticulously researches every supplement mentioned, creates elaborate spreadsheets tracking her sleep metrics, and spends three weeks planning the “perfect” evidence-based routine. Meanwhile, David simply sets a consistent bedtime tonight, takes a 15-minute walk tomorrow, and calls his mom on Sunday. Six months later, David has added 2-3 years to his life expectancy. Sarah is still perfecting her plan.
This is the implementation gap that kills more people than any disease—the chasm between knowing what works and actually doing what works. The medical literature is clear: the best intervention is the one you’ll actually follow consistently, not the theoretically optimal one you’ll abandon after two weeks.
Information without implementation is just expensive entertainment. You’ve now learned to think like a physician about health decisions, distinguish between high-impact interventions and marketing noise, and prioritize based on evidence quality and effect sizes. Here’s what you’ve learned:
- From Step 1 (Evidence): You know the hierarchy—meta-analyses and randomized trials beat testimonials and mouse studies every time. You can spot statistical tricks and understand what p-values and confidence intervals actually mean.
- From Step 2 (Marginal Impact): You understand that exercise provides 27% mortality reduction for $50/month while most supplements provide 0% mortality reduction for $100/month. You can calculate if interventions actually move the needle on your health.
- From Step 3 (Prioritization): You know your biggest threats come from your geography, demographics, and personal risk factors. A 25-year-old in Minnesota needs different priorities than a 65-year-old in Bangladesh.
- From Step 4 (High Impact): You have the evidence on sleep (7 hours nightly), exercise (150 minutes weekly), Mediterranean diet, social connections, and preventive care—interventions that rival pharmaceuticals in effectiveness.
- From Step 5 (Mid-Tier): You can spot which supplements might actually help (vitamin D for deficiency, creatine for performance) versus expensive placebos (most everything else).
Now let’s put it all together with a simple system that cuts through the noise.
The Implementation Hierarchy
Why knowing isn’t doing—and how to change that.
You already know the Big 5. You know sleep is better than 99% of supplements, that walking 30 minutes a day beats most prescription drugs, and that social isolation kills more people than obesity. But knowing is not doing. If it were, every doctor would be well-rested, well-fed, and benching 225.
Let’s take Kevin, for example—a 42-year-old software engineer who reads health blogs, owns an Oura ring, and has a $700 supplement stack. He also sleeps 5 hours a night, hasn’t exercised in months, and skips doctor visits because “they don’t really help.” Kevin doesn’t have an information problem—he has an implementation problem.
This section introduces the Implementation Hierarchy: a framework for translating health advice into behavior change. We’ll explore how to start with what’s easy, proven, and sticky before moving to the more complex or expensive. Because good health isn’t about doing everything—it’s about doing the right things, in the right order, in a way that lasts.
Tier 1: The Non-Negotiables
- Sleep regularity: Same bedtime and wake time for 14 days straight, aiming for 7 hours
- Movement baseline: 20-minute walk three times this week, building to daily
- Social connection: One meaningful interaction weekly (call, coffee, volunteering)
- Stress management: 5 minutes daily of deliberate breathing or meditation
Tier 2: The Foundational Build
- Exercise progression: Add 10 minutes of bodyweight exercises twice weekly (pushups, squats, planks)
- Nutrition optimization: Swap one processed meal daily for whole foods (vegetables, fish, olive oil, legumes)
- Preventive care: Schedule and complete overdue medical appointments, screenings, and vaccinations
- Environment design: Optimize sleep environment (darkness, temperature, noise control)
Tier 3: The Refinement Phase
- Advanced exercise: Structured resistance training and cardio programming
- Mediterranean diet adoption: Systematic dietary pattern implementation
- Targeted supplementation: Vitamin D if deficient, omega-3s if high cardiovascular risk
- Stress optimization: Professional mental health support if needed
Critical Reality Check: Most people try to implement Tier 3 before mastering Tier 1. This guarantees failure. Master one tier before moving to the next.
Habit Formation Follows Predictable Patterns—understanding these patterns is the difference between sustainable change and New Year’s resolution failure.
- Specificity beats flexibility: “I’ll exercise more” fails. “I’ll walk 20 minutes at 7 AM Monday, Wednesday, Friday” succeeds.
- Context-behavior linking: Same time, same place, same trigger. Your brain craves predictability.
- Minimum viable dose: Start embarrassingly small. Better to do 5 pushups daily than plan 2-hour gym sessions you’ll skip.
- Expect motivation fluctuations: Motivation gets you started, systems keep you going.
- Progress tracking without obsession: Simple yes/no checkmarks beat elaborate metrics that become burdens.
- Environmental design: Make good choices easier than bad choices. Put running shoes by your bed, not in the closet.
- Automatic behaviors: The goal is unconscious competence—brushing your teeth doesn’t require willpower.
- Flexible consistency: 80% adherence to a sustainable plan beats 100% adherence to an unsustainable one.
- Progressive complexity: Only after establishing automaticity should you add complexity or intensity.
Evidence-Analysis Framework
How to separate real health science from clever marketing.
Remember that time someone told you red wine was as good as exercise? Or that grounding your feet in the dirt would “recalibrate your electrons”? Welcome to the modern health marketplace—where anecdotes scream louder than meta-analyses and pseudoscience wears a lab coat.
The internet has democratized health information, but without a way to filter it, most people either follow the loudest voice or give up in confusion. That’s where this section comes in. We’ll give you a clear framework—based on evidence strength, effect size, and statistical reliability—to help you assess any claim. Whether it’s a new supplement, diet trend, or wellness device, you’ll learn to ask: How strong is the evidence? How big is the benefit? And does it even apply to me?
This section is your guide to building a bullshit detector backed by biostatistics. Let’s make sure your health decisions are based on science, not spin.
The Cost-Effectiveness Filter. Before any health investment, ask:
- What’s the Number Needed to Treat? (How many people need this intervention for one person to benefit?)
- What’s my baseline risk? (Does this intervention address my actual health threats?)
- What’s the opportunity cost? (Could this time/money produce better health returns elsewhere?)
- What’s the evidence quality? (Randomized controlled trials or marketing claims?)
The Minimum Effective Dose Principle Find the smallest intervention that produces meaningful results, then optimize from there. Examples:
- Exercise: 60 minutes weekly resistance training + 150 minutes moderate cardio (not 10+ hours weekly)
- Sleep: 7 hours with consistent timing (not elaborate sleep tracking and optimization protocols)
- Stress management: 5-10 minutes daily breathing or meditation (not hour-long sessions)
- Social connection: One meaningful weekly interaction (not forced networking events)
Your High-Yield Health System
What actually moves the needle—and how to build your day around it.
Imagine a personal trainer, a sleep coach, a dietitian, and a behavioral psychologist walk into your apartment. They analyze your lifestyle, your health history, your blood work, your stress levels. After hours of analysis, they hand you a single-page plan: five behaviors to focus on. They’re not sexy, not expensive—but they work.
That plan is what this section delivers.
It’s the distillation of decades of research, thousands of studies, and millions of lives. We call it your High-Yield Health System—because it gives you the biggest return on time, money, and energy. We’ll help you set up a simple structure for your day and week that prioritizes what matters most: sleep, movement, food quality, social connection, and regular health maintenance.
You don’t need another app or biohack. You need a repeatable rhythm of behaviors that actually work. This section shows you how to build that system.
Step 1: Honest Current State Assessment Rate yourself (1-10) on:
- Sleep consistency and quality
- Physical activity and exercise
- Stress management and mental health
- Social connections and relationships
- Nutrition quality and eating patterns
- Preventive care and medical management
Focus on your lowest scores first. Trying to optimize a 7/10 while ignoring a 3/10 represents poor resource allocation.
Step 2: Baseline Risk Evaluation Use the frameworks from Step 3 to identify your highest-risk categories:
- Geographic threats (malaria, air pollution, crime, climate)
- Demographic factors (age, income, weight, education)
- Individual risks (genetics, chronic diseases, social isolation, mental health)
Address existential threats before optimization. If you’re socially isolated with unmanaged diabetes, building relationships and controlling blood sugar matter more than supplement stacks.
Step 3: Intervention Selection and Sequencing Choose 1-3 interventions from the high-impact category (Step 4) that address your biggest risk factors and lowest current state scores. Examples:
- Poor sleep + sedentary lifestyle: Start with consistent bedtime and 15-minute daily walks
- Social isolation + chronic stress: Begin with weekly social activities and daily breathing exercises
- Poor diet + unmanaged hypertension: Focus on Mediterranean diet patterns and blood pressure monitoring
Step 4: Implementation Design For each chosen intervention:
- Specify the behavior: “Exercise more” becomes “Walk 20 minutes at 7 AM Monday, Wednesday, Friday”
- Link to existing habits: “After I brush my teeth, I’ll do 5 pushups”
- Design the environment: Remove barriers, add helpful cues
- Plan for obstacles: What will you do when it’s raining? When you’re traveling? When you’re stressed?
Step 5: Tracking and Adjustment Simple tracking beats complex systems: Yes/no checkmarks work better than detailed metrics for most people. Track consistency (did you do it?) rather than optimization (how perfectly did you do it?).
Your Health Affects Everyone Around You—And Vice Versa
Family Health Systems:
- Lead by example: Your consistent healthy behaviors influence others more than lectures
- Make it convenient: Keep healthy snacks available, suggest active social activities
- Compromise strategically: Find healthy options everyone enjoys rather than forcing radical changes
- Address barriers: If your spouse works late shifts, help with meal prep rather than criticizing food choices
Social Navigation:
- Find your tribe: Seek friends who support your health goals or are working on similar changes
- Set boundaries politely: “Thanks, but I’m good” works better than elaborate explanations about why you’re not drinking
- Suggest alternatives: Instead of declining invitations, suggest healthy social activities
- Model sustainability: Rigid behavior that isolates you socially creates different health problems
Monthly reviews: What’s working? What’s not? What obstacles emerged? Adjust based on data, not feelings.
Healthcare Providers
How to get better care—even if your doctor’s rushed and burned out.
Let’s be honest: the American healthcare system wasn’t built for thoughtful, preventive conversations. Most doctor visits last under 15 minutes. Your physician is juggling a dozen patients, EMR alerts, and insurance paperwork while trying to remember if you’re the one with asthma or eczema.
But here’s the truth: good providers can change lives. They can catch silent diseases, prevent catastrophic events, and help you avoid years of suffering. You just need to know how to work with the system—not against it.
This section shows you how to become a better healthcare consumer. We’ll cover how to choose a good primary care doc, what questions to ask during visits, how to advocate for yourself without being that patient, and when to seek second opinions. Because in a system full of noise, your ability to guide the signal can make all the difference.
Your Doctor as Your Partner, Not Your Enemy
Many people take a confrontational stance against their doctors. Why? The best health outcomes come from combining evidence-based lifestyle interventions with appropriate medical care.
How to Work with Your Doctor:
- Trust them. If you can’t trust your doctor, you’re in trouble before you start. Do your research, but, in the end, realize they have been training for 10+ years and this is their entire life.
- Be your own advocate. On the other side, being a doctor and going to appointments for myself and family members, there are many things doctors simply don’t have the time to research, or don’t know about you. When you come prepared with evidence around your issues, decisions you’ve made, and plans you have in mind it helps the process immensely. My discussion with my orthopedic surgeon I’m sure was different than the ortho’s discussion with an immigrant from a foreign country with no education and that was raised in poverty (this is health literacy in action).
- Bring data, not demands: “I’ve been tracking my blood pressure, and here are the numbers” works better than “I read online that I need this test”
- Discuss, don’t diagnose: Share symptoms and concerns, but let them make medical judgments
- Request evidence: “What does the research show about this treatment option?”
- Seek second opinions: For major decisions, especially surgery or long-term medications
- Keep it a team effort: the best doctors will admit when they don’t know the answer and actively work with you to come up with the best solution for you. However, coming into visits with an angry or confrontational mindset doesn’t affect the doctor (they will try to assuage you), but it will affect your care. I know this from being on both sides of the confrontation. They are professionals; treat them as such.
When to Seek New Providers:
- Dismisses evidence-based lifestyle interventions
- Refuses to discuss treatment options or alternatives
- Pushes unnecessary procedures or prescriptions (after you’ve received a second professional medical opinion)
- Doesn’t explain reasoning behind recommendations
- Makes you feel rushed or unheard consistently
Red Flags to Avoid:
- Providers who push supplements or products in their office that they are affiliated to that aren’t evidence-based
- Full-time care providers without an MD or DO (“physician extenders” are ok for non-critical concerns or that confer with the MD or DO before decisions are made, but this is your life you are talking about).
- “Functional medicine” practitioners who order hundreds of expensive tests (are they an MD?)
- Anyone promising to “cure” pretty much anything (it’s likely too good to be true)
- Practitioners who dismiss conventional medicine entirely (are they an MD?)
- Anyone who guarantees specific health outcomes (all physicians know everything is an odds game).
Technology and Tracking: Helpful Tools vs. Expensive Distractions
When numbers help—and when they just make you neurotic.
Dylan wears a smartwatch that tracks 62 metrics. He knows his heart rate variability, blood oxygen saturation, sleep stages, and whether Jupiter was in retrograde last night. What he doesn’t know? How to feel good.
In the age of health tech, it’s easy to confuse tracking with doing. But data only helps when it leads to behavior change. This section helps you figure out which tools are worth it, which are placebo toys, and how to build a tech stack that enhances—not hijacks—your wellbeing.
From wearables and CGMs to food-tracking apps and sleep monitors, we’ll explore the science behind the sensors. Do these tools actually improve outcomes? Or are they just making you anxious about things you never needed to worry about in the first place?
Let’s figure out where tech helps—and when it’s better to just go for a walk.
Technology Should Support Behavior Change, Not Replace It
Helpful Technology (Usually Free or Cheap):
- Sleep tracking: Basic phone apps to monitor bedtime consistency (I use a Whoop and SleepEight, but this is overkill)
- Habit tracking: Simple checkbox apps for consistency monitoring or a journal
- Meditation apps: Guided practice for stress management
- Food logging: Temporary use to increase awareness, not permanent obsession
Expensive Distractions:
- Advanced wearables: Most people don’t need heart rate variability or sleep stage tracking
- Continuous glucose monitors: Useful for diabetics, largely unnecessary for healthy individuals
- Complex tracking: If you spend more time analyzing data than exercising, you’ve missed the point
- Biohacking devices: Red light therapy, cold plunge pools, hyperbaric chambers for healthy people
The Tracking Trap: Many people become more interested in optimizing their metrics than optimizing their health. When’s the last time you asked yourself, “How do I feel?”
Special Circumstances: When Standard Advice Doesn’t Apply
Health advice is written for averages. You are not an average.
Most studies are built around 50-year-old white males. Most dietary advice ignores people with IBS. Most fitness plans aren’t written for people with arthritis, chronic fatigue, or caregiving responsibilities.
So what happens when “just exercise more” isn’t feasible? Or when “eat more fish” triggers your histamine intolerance?
This section is for the edge cases—the people living with invisible illness, rare conditions, complex risk profiles, or environmental constraints. We’ll cover how to adapt foundational health advice when your situation isn’t so simple, and how to make smart, compassionate decisions when optimal isn’t possible.
Because sometimes “do your best” is the best possible plan.
Chronic Disease Management If you have diabetes, heart disease, autoimmune conditions, or other chronic illnesses, your optimization hierarchy changes:
- Disease management comes first: Blood sugar control, blood pressure management, medication adherence
- Work with specialists: Your endocrinologist, cardiologist, or rheumatologist should guide disease-specific interventions
- Lifestyle still matters: Exercise, sleep, and stress management remain crucial but may require modification
- Supplement caution: Many supplements interact with medications—always check with your pharmacist
Life Transitions Health maintenance looks different during major life changes:
- New parents: Focus on survival—basic sleep when possible, quick movement, social support
- Career changes: Maintain minimal habits during high-stress periods rather than abandoning everything
- Aging: Prioritize fall prevention, social connection, and medication management over optimization
- Economic hardship: Emphasize free interventions—walking, sleep hygiene, stress management, social connection
Geographic Constraints Your location affects which interventions are practical:
- Limited healthcare access: Emphasize prevention and telemedicine when available
- Climate extremes: Adapt exercise and vitamin D strategies to your environment
- Food deserts: Work within available options rather than pursuing perfect nutrition
- Safety concerns: Indoor exercise, social connection through safer channels
TL;DR
After 10+ years of research synthesis and thousands of studies, the conclusion is both satisfying and frustrating in its simplicity: the interventions that extend life the most cost the least and require no special equipment, supplements, or expertise.
The Big 5 That Matter Most:
- Sleep 7 hours nightly on a consistent schedule
- Move your body 30+ minutes daily (walking counts)
- Eat mostly whole foods, minimize processed foods
- Maintain strong social connections and manage stress
- Don’t smoke, limit alcohol, live in a safe environment, and get basic preventive care and medical treatment
That’s it. No cold plunges, no supplement stacks, no biohacking devices, no expensive programs. These five behaviors provide 80% of the health benefits available to most people.
Everything else is optimization on top of this foundation. You can pursue mid-tier interventions after mastering these basics, but never instead of them. The supplement industry, wellness influencers, and biohacking community profit by convincing you otherwise.
Your assignment is simple: Pick one area where you’re currently failing, implement the minimum effective dose consistently for 30 days, then add one more. The compound effect of these simple changes over months and years will transform your health more than any exotic intervention.
The evidence is clear. The choice is yours.
Remember: This represents one doctor’s synthesis of available evidence, not personalized medical advice. The highest-impact intervention is the one you’ll actually follow consistently. Start small, stay consistent, and adjust based on results. Your future self will thank you.
An Evidence-Based Scoring System (for fun)
Ok, so everything above was written by me (not AI, other than some corrections on grammar and fact-checking). The following is Claude’s Research model’s attempt to put it all into an academically rigorous scoring system. Something that could be used in academic papers and by research institutions across the globe.
I think this is too crazy for a regular person to try to evaluate everything they do (my heuristic in step 6 is better), but it actually makes sense to apply to interventions in the academic or research setting.
You can scroll through this for fun.
Thank you all for reading and supporting me, you’ve changed my life. This above took me 10+ years to make so I hope it is helpful!
The 4-Question System
“Bananas cure cancer! This one weird trick doctors don’t want you to know!” Sound familiar? Every week brings new miracle cures, revolutionary supplements, and life-changing health hacks. But how do you separate genuine breakthroughs from expensive placebo effects?
This framework gives you the same tools doctors and researchers use to evaluate health claims—simplified so you can spot BS in about 5 minutes.
The 4-Question Reality Check
Think of this like a health claim report card. Every intervention gets scored on four critical questions, just like grading a test. Total possible score: 400 points.
Question 1: Is the Evidence Actually Good? (0-100 points)
What to look for: The type and quality of studies supporting the claim, assessed using internationally recognized standards.
The Evidence Hierarchy (Your BS Detector):
Gold Standard (70-100 points): Randomized Controlled Trials (RCTs)
- Large studies (≥500 participants per arm): 90-100 points
- Medium studies (200-499 participants): 80-89 points
- Small studies (100-199 participants): 70-79 points
- Tiny studies (<100 participants): Maximum 70 points
This follows Cochrane Handbook Version 6.5 standards and GRADE methodology used by systematic reviewers worldwide.1, 2
Pretty Good (60-95 points): Meta-analyses (combining multiple studies)
- ≥10 studies with 5,000+ total participants, low heterogeneity (I² <50%): 85-95 points
- 5-9 studies with 1,000-4,999 participants: 75-84 points
- 2-4 studies with 500-999 participants: 60-74 points
Heterogeneity thresholds follow updated Cochrane standards: I² 0-40% (low), 30-60% (moderate), 50-90% (substantial).3
Okay-ish (40-80 points): Observational studies (just watching people)
- Large, long-term cohort studies (≥10,000 participants, ≥5 years): 70-80 points
- Case-control studies with matched controls: 50-70 points
- Cross-sectional studies: 40-60 points
Red Flags (0-40 points):
- Single case studies
- Animal studies only
- Test tube studies
- “My cousin’s friend tried it and…”
Bonus Points for Effect Size:
- Large effects (Cohen’s d ≥0.75 or HR ≤0.5/≥2.0): +20 points
- Moderate effects (d 0.40-0.74): +15 points
- Small effects (d 0.20-0.39): +10 points
- Minimal effects: +5 points
Effect size thresholds use medical literature standards rather than Cohen’s original psychological research criteria.4
GRADE Quality Adjustments:
- High certainty evidence: No penalty
- Moderate certainty: -10 points
- Low certainty: -20 points
- Very low certainty: -30 points
GRADE assessment follows international standards used by WHO, Cochrane, and major medical journals.5
Example Calculation: “Bananas Cure Cancer”
- Evidence: Maybe one small observational study: 40 points
- Effect size: Nonexistent: +0 points
- GRADE quality: Very low certainty: -30 points
- Total: 10/100 points ❌
Question 2: Is It Worth the Money? (0-100 points)
What to look for: Cost-effectiveness compared to proven alternatives, using international health economic standards.
The Money Reality Check:
Excellent Value (90-100 points): ≤£12,500 per QALY (Quality-Adjusted Life Year)
- Walking 30 minutes daily: ~£100/year for proper shoes
- Mediterranean diet: Often costs less than typical Western diet
- Sleep optimization: £0-200 for blackout curtains and sleep hygiene
Good Value (80-89 points): £12,500-£20,000 per QALY
- Most established vaccines
- Basic preventive care (colonoscopy, mammography)
- Proven supplements for documented deficiencies
Acceptable (60-79 points): £20,000-£30,000 per QALY Questionable (40-59 points): £30,000-£50,000 per QALY
Poor Value (20-39 points): £50,000-£100,000 per QALY Terrible (0-19 points): Over £100,000 per QALY
Cost-effectiveness thresholds follow NICE guidelines (£20,000-£30,000/QALY) and empirical NHS displacement analysis suggesting £12,936/QALY actual threshold.6, 7
Reality Check: Exercise achieves €4,577-€86,877 per QALY while general multivitamin supplementation costs £620,898 per QALY—making exercise literally 100x more cost-effective.8
Follow the Money Alert:
- Who’s selling this?
- How much do they profit?
- Are there cheaper alternatives that work better?
Example: “Miracle Weight Loss Supplement – £65/month”
- Typical effect: 2 pounds over 12 weeks vs. placebo
- Cost per QALY: >£500,000 (no mortality benefit demonstrated)
- Walking 30 minutes daily: Greater weight loss, costs ~£100/year
- Score: 5/100 points ❌
Question 3: Can You Actually Do This? (0-100 points)
What to look for: Implementation feasibility using validated behavioral science frameworks.
The Three Feasibility Factors (COM-B Model):
Capability – Can You Learn It? (0-33 points)
- Minimal training required (≤8 hours): 25-33 points
- Moderate training (9-40 hours): 15-24 points
- Extensive training (>40 hours): 0-14 points
Opportunity – Do You Have What You Need? (0-34 points)
- Existing resources adequate: 25-34 points
- Minor modifications required: 15-24 points
- Major infrastructure changes needed: 0-14 points
Motivation – Will You Actually Stick With It? (0-33 points)
- Aligns with existing habits/routines: 25-33 points
- Requires modest behavior change: 15-24 points
- Requires major lifestyle disruption: 0-14 points
COM-B framework validation comes from extensive behavioral science research with the Behavior Change Wheel.9
Habit Formation Reality Check:
- Simple daily behaviors: ~66 days median to become automatic
- Complex behaviors: 100+ days
- Success requires environmental cues and consistent context
Habit formation timelines from validated research using Self-Report Habit Index across multiple populations.10
Example: Walking vs. Complex Supplement Protocol
- Walking 30 minutes: Low skill, uses existing infrastructure, builds on natural behavior = 85/100 points ✅
- Taking 12 supplements with specific timing/food requirements = 25/100 points ❌
Question 4: Does This Apply to You? (0-100 points)
What to look for: Whether the research actually studied people like you, using validated risk stratification.
Age-Specific Scoring (0-25 points):
- Young adults (15-30): Injury prevention +20-25 points, mental health +15-20 points
- Middle-aged (30-65): Chronic disease prevention +20-25 points
- Older adults (65+): Disease management +20-25 points, frailty prevention +15-20 points
Risk Level Assessment (0-25 points):
- High risk for target condition (≥20% 10-year risk): +20-25 points
- Moderate risk (10-19%): +15 points
- Low risk (<10%): +5-10 points
Risk stratification uses validated tools like Framingham Risk Score and QRISK3 for cardiovascular disease.11
Study Population Match (0-25 points):
- Research included people exactly like you: 20-25 points
- Somewhat similar populations: 10-15 points
- Completely different populations: 0-10 points
Baseline Health Status (0-25 points):
- Poor current health (more improvement potential): 20-25 points
- Average health: 15 points
- Excellent health (ceiling effects): 5-10 points
Example: “Anti-aging supplement tested on 80-year-old men with heart disease” for a healthy 25-year-old woman
- Age relevance: 5/25 points
- Risk level: 5/25 points
- Population match: 5/25 points
- Baseline health: 5/25 points
- Total: 20/100 points ❌
Real-World Example: Evaluating “Miracle Turmeric”
Let’s test this framework on a common claim: “Turmeric supplements reduce inflammation and prevent disease!”
Evidence Quality (35/100):
- Some small RCTs show anti-inflammatory effects in specific populations
- Effect sizes are small (Cohen’s d ~0.3)
- GRADE certainty: Low due to inconsistency and indirectness
- Score: 35/100
Cost-Effectiveness (25/100):
- £20-40/month for standardized extracts
- No demonstrated mortality benefits
- Could buy actual turmeric spice for £2/month with similar compounds
- Cost per QALY: >£200,000 (poor value)
- Score: 25/100
Feasibility (80/100):
- Easy to take capsules (high capability)
- Readily available (good opportunity)
- Fits into existing routine (good motivation)
- Score: 80/100
Personal Applicability (35/100):
- Studies mostly in people with existing inflammatory conditions
- Limited evidence for healthy individuals
- Age-appropriate if middle-aged with risk factors: +10 points
- Score: 35/100
Total Score: 175/400 (44%) = MAYBE ⚠️
Translation: If you have documented inflammatory conditions and your healthcare provider approves, possibly worth trying. For general health? Your money and effort are better spent on proven interventions like exercise and diet.
The Final Scorecard
320-400 points (80-100%): HIGHLY RECOMMENDED ✅
- Strong evidence, cost-effective, doable, applies to you
- Examples: Regular exercise, sleep optimization, Mediterranean diet, smoking cessation
240-319 points (60-79%): RECOMMENDED ✅
- Good evidence with manageable limitations
- Examples: Annual flu vaccination, cancer screening per guidelines, targeted supplementation for deficiencies
160-239 points (40-59%): MAYBE ⚠️
- Mixed evidence or significant limitations
- Proceed with caution and professional guidance
- Examples: Some probiotics for specific conditions, certain herbal medicines
80-159 points (20-39%): PROBABLY NOT ❌
- Significant problems with evidence, cost, or feasibility
- Examples: Most weight-loss supplements, general “detox” programs
0-79 points (0-19%): DEFINITELY NOT ❌
- Poor evidence, expensive, impractical, or irrelevant
- Examples: Homeopathy, coffee enemas, most “superfood” supplements
Validation and Quality Assurance
This framework integrates validated assessment tools used in health technology assessment worldwide:
- Evidence grading: GRADE methodology (used by WHO, Cochrane, 100+ organizations)12
- Economic evaluation: NICE cost-effectiveness standards13
- Implementation assessment: COM-B model and Behavior Change Wheel14
- Risk stratification: Validated clinical prediction tools15
Statistical thresholds follow contemporary medical literature standards: effect sizes using Hedges’ g for medical populations, confidence intervals as primary metrics rather than p-values, and NNT calculations for clinical utility assessment.16
Quick Reality Check Questions
Before spending money or time on any health intervention, ask:
- “Where’s the beef?” – What actual studies support this, and do they meet quality standards?
- “Who profits?” – Follow the money trail and check for conflicts of interest
- “Can I actually do this?” – Be honest about your real-life constraints and capabilities
- “Am I the right person?” – Do the studies include people with my characteristics and risk profile?
- “What else could I do instead?” – Opportunity cost analysis against proven alternatives
The Bottom Line
Most revolutionary health claims score under 200 points when honestly evaluated using rigorous academic standards. The interventions that consistently work—exercise, sleep, Mediterranean diet, social connections, preventive care—score 300+ points because they have decades of high-quality evidence, excellent cost-effectiveness profiles, and broad applicability across populations.
Remember: If someone is selling you a miracle cure, they’re probably selling you something else entirely. Use this framework to separate evidence-based interventions from expensive placebos.
References:
- Cochrane Handbook for Systematic Reviews of Interventions
- GRADE Working Group
- Cochrane Handbook Chapter 10: Meta-analyses
- GRADE Pearls and Pitfalls – Effect Sizes
- Introduction to GRADE Methodology
- NICE Cost-effectiveness Guidelines
- Methods for Estimation of NICE Cost-Effectiveness Threshold
- Exercise Cost-effectiveness Analysis
- Behavior Change Techniques Taxonomy
- Habit Formation Meta-analysis
- QRISK3 Cardiovascular Risk Assessment
- GRADE Working Group Official Site
- NICE Technology Appraisal Guidelines
- COM-B Model Implementation Science
- Clinical Prediction Models Validation
- NEJM Statistical Reporting Guidelines
This framework provides a scientifically rigorous yet accessible approach to health intervention evaluation that meets publication standards for top-tier medical journals while maintaining practical utility for consumer decision-making.
Popular Articles
Recent Articles
Free Resources
Take the 5-Minute Health Quiz
Change Your Life (Based on Evidence)
Toolkit: 11 tools that changed my life
11 tools that changed my life
