
What happens to your body when you don’t eat? You might experience headaches, ketogenesis, or even psychosis. How long until you die? Is there any benefit to fasting really?
Millions of humans have fasted repeatedly through Ramadan, Yom Kippur, or hunger strikes. More and more people are trying intermittent fasting, where they don’t eat for 8 hours during the day or even a week at a time. What is going on here? Is this science or nonsense? And what does not eating for an hour, a day, or a year do to your body?
Well, I am a doctor, but I need clarification. There is evidence everywhere; some sources say fasting will kill you, but also fasting will help you live longer. These quick takes are exciting, but I want to understand:
- What physically happens to the body when you don’t eat
- When do things become dangerous
- What happens when you start eating again after fasting
- Is there any merit to not eating for extended periods of time, for health
Let’s dive deep:
*Importantly, this is simply a deep dive into the science of fasting. Please talk to your doctor before eating 17 pizzas in one hour or fasting until the next eclipse. This is not medical advice.
1. The Energy Cascade
I began by simply figuring out where your body draws energy. I know we need ATP and that ATP typically comes from the breakdown of glucose, but are there other ways to generate ATP? What happens when we run out of glucose?
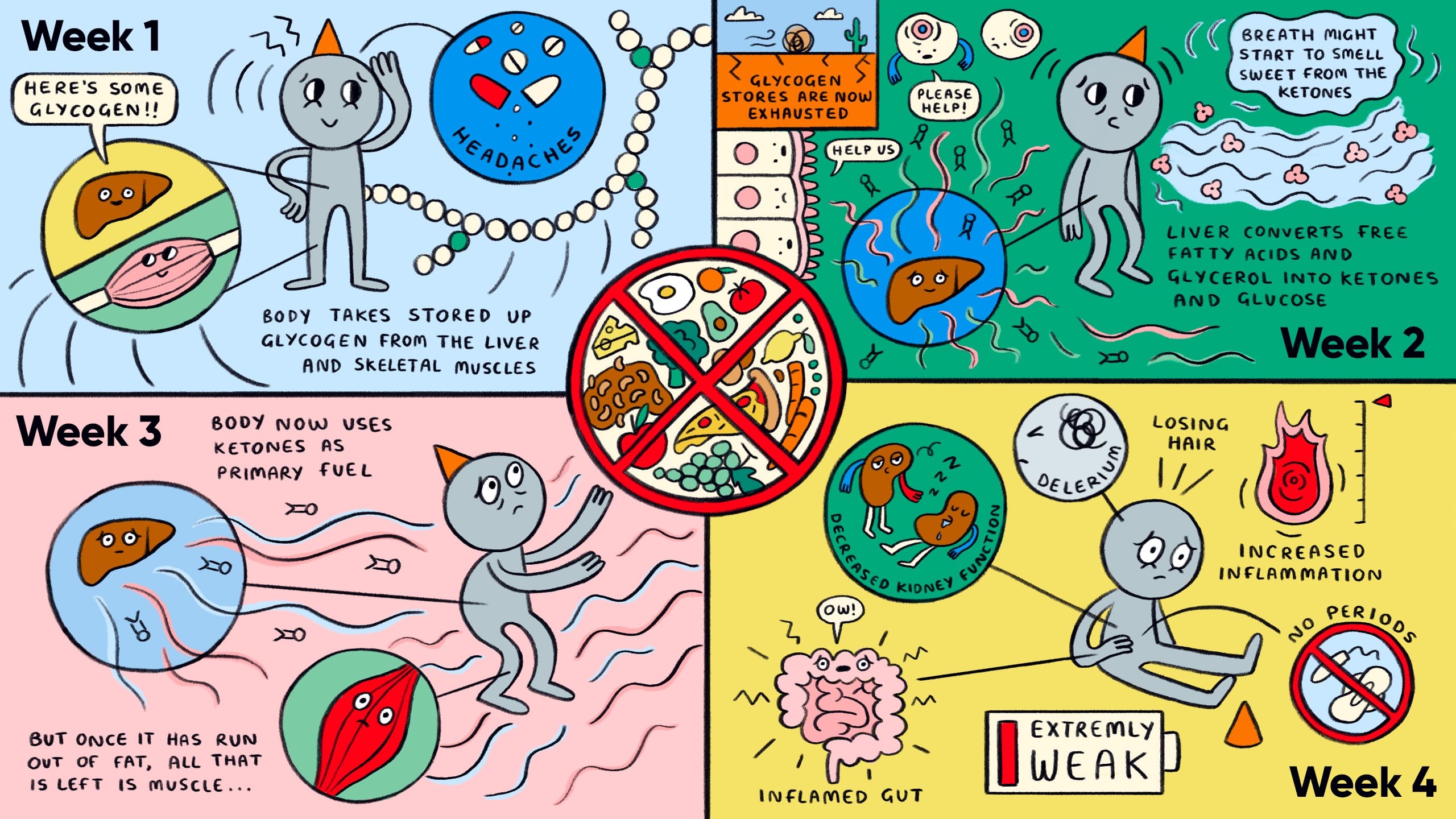
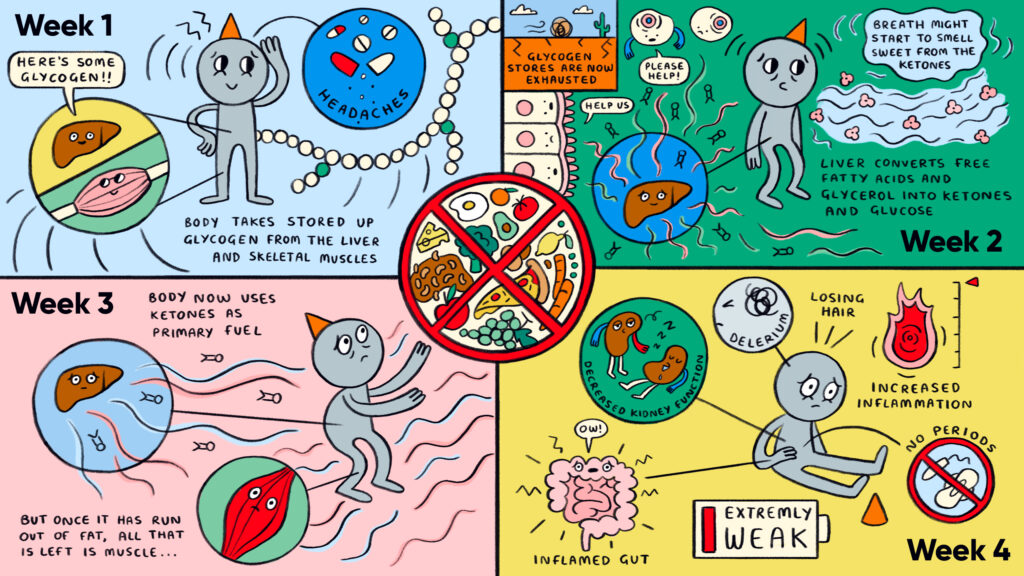
- After 1 Day
- The first thing many people notice is a headache.4 Your body usually uses glucose in the blood to generate energy for your cells through glycolysis (breaking glucose down to provide energy, ATP). Without this energy, cells will break down and die or can’t function properly to do what you do to live, such as move your muscles or think. Cells may use energy to maintain the perfect balance of sodium and potassium in the cell or make proteins.
- Glycogen in the liver and skeletal muscle is the first place your body turns to replete that blood glucose. Glycogen is simply a chain of glucose and can be quickly and efficiently broken down to replete your blood glucose stores.5,6 This is why people carb-load the day before a big marathon; they want to make sure those glycogen stores are as big as possible.
- After 2-3 Days
- Goodbye glycogen, hello fat and protein. If we are undergoing intense exercise, we can exhaust our glycogen stores as soon as ~80 minutes into intense exercise.
- At rest, each muscle cell contains roughly 1 billion ATP molecules, all of which will be used and replaced every 2 minutes; during intense exercise, muscle ATP production can increase 1000-fold to meet the demands of intense muscle contraction.7
- At this point, our body is going into overdrive to generate glucose so our body’s cells can stay alive. So we can think, move, and breathe.
- Triglycerides (fats) are separated into free fatty acids and glycerol in the body that the liver converts into ketone bodies and glucose (your breath might start to smell sweet! That’s the ketones; in diabetes, this is a sign that someone might be severely hypoglycemic).
- Proteins start to break down. Special amino acids are pulled into the fray; some are ketogenic, and some are glucogenic. All are trying to generate energy for your cells; therefore, you don’t kick the bucket.
- Around this point, we will likely notice confusion, sleepiness, muscle spasms, and GI upset.
- At one Week
- Your body is well-versed in using ketones for energy at this point. You might be in a state of true ketosis by four days in which the body uses triglycerides (fats) as the primary fuel source instead of carbohydrates (like sugar). However, given that we aren’t supplementing our diet with fats, our bodies also turn to protein to help generate energy. And once our fat is depleted, muscle is all that’s left.
- >Two Weeks
- At around ten days, the body can show an increased release of systemic inflammatory markers and decreased kidney function. 2,3
- After two weeks, chances of severe neurological and physiological changes increase, such as delirium, psychotic episodes, renal failure, colitis (inflammation of the gut), Wernicke-Korsakoff syndrome, and more.9,10
- When malnourishment hits, we could start losing hair and muscle, stop having periods (women), and become extremely weak.26 This level of fasting is extremely difficult and usually dangerous.
Overall, the evidence points to extended periods of fasting, >10 days, being harmful nearly always, with the most dangerous time starting when your body starts to consume protein.
2. Death by starvation
But when do you die?
Most people can survive at least 30 days without food. However, after that, things get tricky:
- How old are you? Children will die much more quickly without food. The underweight elderly are also particularly at risk.
- What’s your current BMI? One study reveals lean people can lose around 18% of their body mass while fasting before suffering severe consequences, while obese people might be able to tolerate >20%.1
- Are you male or female? Females usually live longer.27
- Do you have adequate access to water? Without it, you will likely perish in 3 days.
Death is generally caused by an electrolyte or acid/base imbalance after your cells can’t function due to a lack of energy, causing them to lyse (explode), removing any functionality they had and releasing the contents of the cell to the rest of the body. For example, suppose your heart muscle cells can’t function or conduct electricity correctly. In that case, they can’t coordinate the squeezing of oxygenated blood into your body, resulting in a rapid, widespread cellular death.
A normal-weight person, on average, can last 2-3 months without food before death.8,24
Gandhi undertook 17 fasts, with the longest being 21 days.11
The longest recorded fast was Angus Barbieri, a 456-pound 27-year-old Scott who fasted for 382 days. He did, however, have vitamins, electrolytes, and yeast but consumed no calories. At the end of it, he was 180 pounds.
3. Rebound Eating
Refeeding syndrome can kill you. I remember we would see it all the time in the hospital with people peri-ICU.
- Serious Health Consequences: Refeeding syndrome is a life-threatening condition that can occur when severely malnourished people restart eating. It can cause hypophosphatemia, hypokalemia, and hypomagnesemia, which can lead to seizures, arrhythmias, and respiratory distress. This happens when the body has a massive insulin release in response to new food, resulting in extreme electrolyte imbalances. When insulin pushes glucose into cells, it also moves certain electrolytes in and out of the body. This can be so severe patients can die from it, and to prevent it from happening, patients who are known to be malnourished are usually hospitalized before eating to monitor these electrolytes and replete them as needed.
- Return of Weight: In overweight individuals, caloric restriction and weight loss usually do not provide long-term weight loss.25 Current evidence only supports bariatric surgery and GLP-1s for therapy induced longer-term weight loss.28
4. The Reality of Fasting
Is intermittent fasting actually beneficial? I don’t think science knows:
Intermittent Fasting:
- Intermittent fasting is likely a fad with insufficient long-term evidence to support or deny its benefits. Regarding weight loss, biomarkers (such as leptin and cholesterol), and glycemic control, the net energy change seems to be the most crucial difference, with intermittent vs continuous restrictions showing no significant differences.15-17
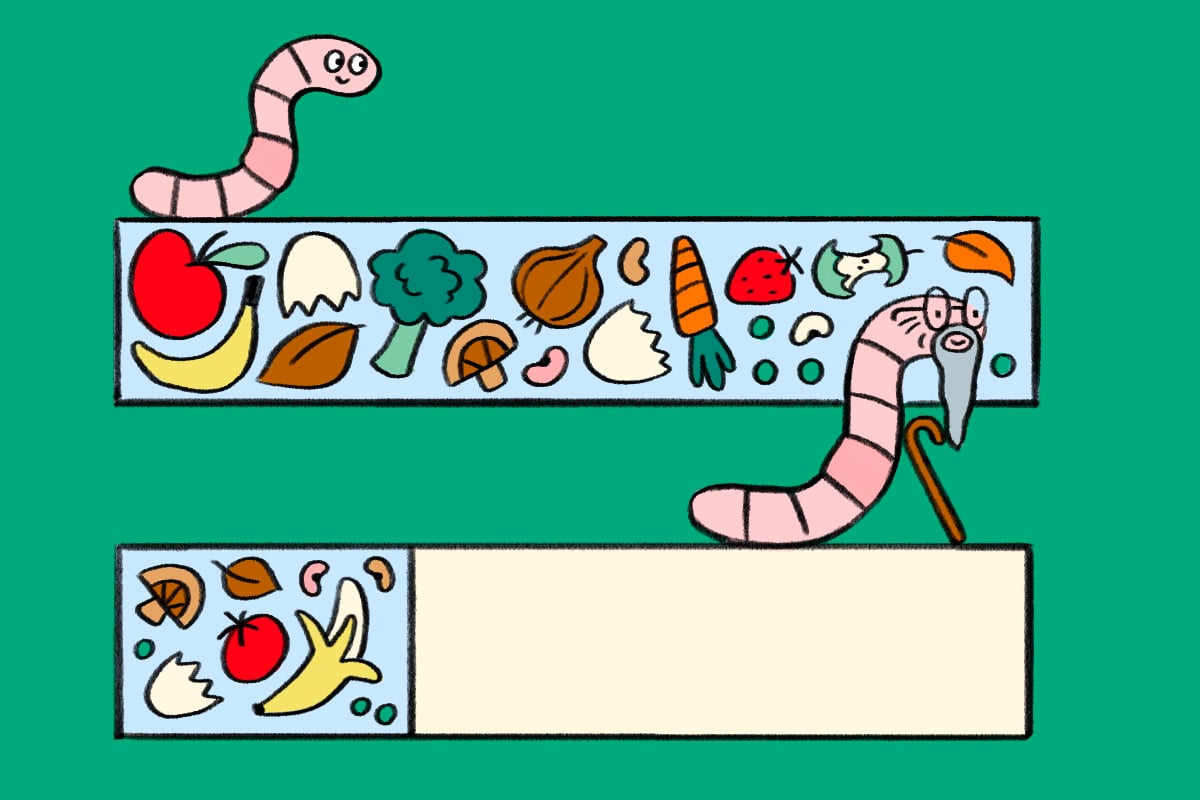
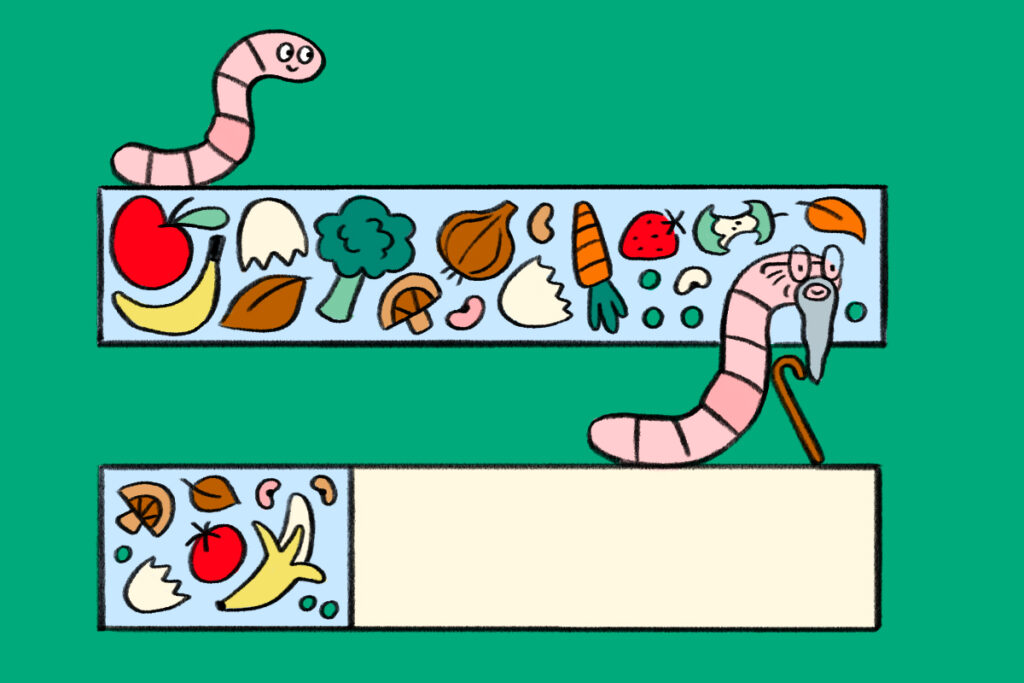
- Some studied benefits include the potential for benefits in neurological diseases, metabolic syndromes, and certain cardiovascular diseases. Two of the most hyped aspects of intermittent fasting are the inhibition of tyrosine kinase enzymes and their benefits in cancer prevention and treatment and the potential “slow-down” of cellular aging as well as simple organisms, like bacteria and worms, living significantly longer when fasting as opposed to being fed.21-23 (If you want to learn more about the possible benefits, source 22 provides an excellent overview).
- Compared to overnight fasting, intermittent fasting triples fluctuations in free fatty acids and induces reductions in insulin sensitivity and acute glucose-simulated insulin response. Why is this important? Decreased insulin sensitivity and lipotoxic mechanisms are thought to cause the development of Type II Diabetes as well as being associated with obesity and cardiovascular disease.19 The most recent “scary” article was from AHA, which looked at 20,000 adults and found that following an 8-hour time-restricted diet had a 91% higher risk of death from cardiovascular disease and that people with heart disease or cancer had a higher risk of cardiovascular death.20
A ketogenic diet:
- A ketogenic diet can have benefits for diabetes, heart disease, obesity, Nonalcoholic fatty liver disease, polycystic ovarian syndrome, neurodegenerative disorders, and cancer.12 However, the possible harmful effects make this a very mixed bag. A proper ketogenic diet seems only to have sufficient evidence for those with epilepsy by increasing the quality of life, seizure severity, and frequency.14
- However, a ketogenic diet can cause issues such as nutrient deficiencies, digestive problems, kidney stones, heart disease, muscle loss, and cognitive decline.13
What do I think? Well, similar to many of my other opinions, moderation is best. Overconsumption often leads to metabolic morbidities (insulin resistance, excessive accumulation of visceral fat, diabetes, cardiovascular risk, etc.), particularly when associated with a sedentary lifestyle. However, underconsumption can lead to bone and muscle loss, decreased primary organ function (kidneys), significant decreases in cognitive abilities, delirium, and death. Proper sleep, exercise, social support, and diet are the levers you want to try and pull here if your goal is weight loss or gain. I try not to eat at least 3 hours before bed, and I also try to maintain a 90% whole foods diet, such as chicken, broccoli, and potatoes.
Summary
- Blood glucose needs to be maintained to energize the cells throughout our body. When it is depleted, we turn to our liver and muscle glycogen stores, then fat and muscle.
- Depending on their state of health, humans can probably live anywhere from 1-3 months without food and adequate water.
- Rebound eating is real and can kill you.
- Intermittent fasting has intermittent benefits. The science isn’t there yet to fully support or deny its benefits.
Sources:
- Elliot B, Mina M, Ferrier C. Complete and voluntary starvation of 50 days. Clin Med Insights Case Rep. 2016;9:67-70. doi:10.4137/CCRep.S39776
- Dai Z, Zhang H, Wu F, Chen Y, Yang C, Wang H, Sui X, Guo Y, Xin B, Guo Z, Xiong J, Wu B, Li Y. Effects of 10-Day Complete Fasting on Physiological Homeostasis, Nutrition and Health Markers in Male Adults. Nutrients. 2022 Sep 18;14(18):3860. doi: 10.3390/nu14183860. PMID: 36145236; PMCID: PMC9503095.
- Fazeli P.K., Zhang Y., O’Keefe J., Pesaresi T., Lun M., Lawney B., Steinhauser M.L. Prolonged fasting drives a program of metabolic inflammation in human adipose tissue. Mol. Metab. 2020;42:101082. doi: 10.1016/j.molmet.2020.101082. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Torelli P, Evangelista A, Bini A, Castellini P, Lambru G, Manzoni GC. Fasting headache: a review of the literature and new hypotheses. Headache. 2009 May;49(5):744-52. [PubMed][Reference list]
- Browning JD, Baxter J, Satapati S, Burgess SC. The effect of short-term fasting on liver and skeletal muscle lipid, glucose, and energy metabolism in healthy women and men. J Lipid Res. 2012 Mar;53(3):577-586. [PMC free article] [PubMed] [Reference list]
- https://www.ncbi.nlm.nih.gov/books/NBK534877/
- Meyer RA, Wiseman RW.. The metabolic systems: control of ATP synthesis in skeletal muscle. In: Farrell PA, Joyner MJ, Caiozzo VJ, ed. ACSM’s Advanced Exercise Physiology. 2nd ed.Philadelphia, PA: Wolters Kluwer; 2012:363–378. [Google Scholar] [Ref list]
- Chalela, J. A., & Lopez, J. I. (2013). Medical management of hunger strikers. Nutrition in Clinical Practice, 28(1), 128–135. 10.1177/0884533612462896 [PubMed] [CrossRef] [Google Scholar] [Ref list]
- Başoğlu M, Yetimalar Y, Gürgör N, Büyükçatalbaş S, Kurt T, Seçil Y, Yeniocak A. (2006). Neurological complications of prolonged hunger strike. Eur J Neurol, 13(10), 1089–15. 10.1111/j.1468-1331.2006.01531.x [PubMed] [CrossRef] [Google Scholar] [Ref list]
- Chalela, J. A., & Lopez, J. I. (2013). Medical management of hunger strikers. Nutrition in Clinical Practice, 28(1), 128–135. 10.1177/0884533612462896 [PubMed] [CrossRef] [Google Scholar] [Ref list]
- Bhargava B, Kant R. Health File of Mahatma Gandhi: His Experiments with Dietetics and Nature Cure. Indian J Med Res. 2019 Jan;149(Suppl):S5-S23. doi: 10.4103/0971-5916.251654. PMID: 31070174; PMCID: PMC6515735.
- Masood W, Annamaraju P, Khan Suheb MZ, et al. Ketogenic Diet. [Updated 2023 Jun 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499830/
- O’Neill B, Raggi P. The ketogenic diet: Pros and cons. Atherosclerosis. 2020 Jan;292:119-126. [PubMed] [Reference list]
- Kverneland M, Molteberg E, Iversen PO, Veierød MB, Taubøll E, Selmer KK, et al. Effect of modified atkins diet in adults with drug-resistant focal epilepsy: a randomized clinical trial. Epilepsia. (2018) 59:1567–76. 10.1111/epi.14457 [PubMed] [CrossRef] [Google Scholar] [Ref list]
- Headland M, Clifton PM, Carter S, Keogh JB. Weight-loss outcomes: a systematic review and meta-analysis of intermittent energy restriction trials lasting a minimum of 6 months.Nutrients. (2016) 8:354–65. 10.3390/nu8060354[PMC free article] [PubMed] [CrossRef] [Google Scholar] [Ref list]
- Harvie MN, Pegington M, Mattson MP, Frystyk J, Dillon B, Evans G, et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers : a randomized trial in young overweight women. Int J Obes. (2011) 35:714–27. 10.1038/ijo.2010.171[PMC free article] [PubMed] [CrossRef] [Google Scholar] [Ref list]
- Cho Y, Hong N, Kim K, Cho SJ, Lee M, Lee Y, et al. The effectiveness of intermittent fasting to reduce body mass index and glucose metabolism: a systematic review and meta-analysis. J Clin Med. (2019) 8:1645–55. 10.3390/jcm8101645 [PMC free article][PubMed] [CrossRef] [Google Scholar] [Ref list]
- Salgin B, Marcovecchio ML, Humphreys SM, Hill N, Chassin LJ, Lunn DJ, et al. Effects of prolonged fasting and sustained lipolysis on insulin secretion and insulin sensitivity in normal subjects. Am J Physiol Endocrinol Metab. (2009) 296:E454–61. 10.1152/ajpendo.90613.2008[PMC free article] [PubMed] [CrossRef] [Google Scholar] [Ref list]
- Salgin B, Marcovecchio ML, Humphreys SM, Hill N, Chassin LJ, Lunn DJ, et al. Effects of prolonged fasting and sustained lipolysis on insulin secretion and insulin sensitivity in normal subjects. Am J Physiol Endocrinol Metab. (2009) 296:E454–61. 10.1152/ajpendo.90613.2008[PMC free article] [PubMed] [CrossRef] [Google Scholar] [Ref list]
- https://newsroom.heart.org/news/8-hour-time-restricted-eating-linked-to-a-91-higher-risk-of-cardiovascular-death
- Longo VD, Mattson MP. Fasting: molecular mechanisms and clinical applications. Cell Metab. 2014 Feb 04;19(2):181-92. [PMC free article] [PubMed] [Reference list]
- Longo, V.D., Di Tano, M., Mattson, M.P. et al. Intermittent and periodic fasting, longevity and disease. Nat Aging 1, 47–59 (2021). https://doi.org/10.1038/s43587-020-00013-3
- Longo VD, Mattson MP. Fasting: molecular mechanisms and clinical applications. Cell Metab. 2014 Feb 4;19(2):181-92. doi: 10.1016/j.cmet.2013.12.008. Epub 2014 Jan 16. PMID: 24440038; PMCID: PMC3946160.
- O’Hagan S. Hunger: the real maze men speak. The Guardian. 2008. Available at: http://www.theguardian.com/film/2008/oct/19/northernireland. [Ref list]
- Tsai AG, Wadden TA. The evolution of very-low-calorie diets: an update and meta-analysis. Obesity (Silver Spring) 2006;14(8):1283–93.[PubMed] [Google Scholar] [Ref list]
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/malnutrition
- Zarulli V, Barthold Jones JA, Oksuzyab A, Lindahl-Jacobsen R, Christensen K, Vaupel JW. Women live longer than men even during severe famines and epidemics. Proc Natl Acad Sci USA. 2018;115(4):E832-E840. doi:10.1073/pnas.1701535115
- Institute of Medicine (US) Subcommittee on Military Weight Management. Weight Management: State of the Science and Opportunities for Military Programs. Washington (DC): National Academies Press (US); 2004. 4, Weight-Loss and Maintenance Strategies. Available from: https://www.ncbi.nlm.nih.gov/books/NBK221839/
